Massive PE Resuscitation
- Oxygen via:
- Nonrebreather @ 15L/min + nasal cannula @ 15L/min
- High flow nasal prongs
- Thrombolysis
- Standard dose: 100 mg alteplase (10-20 mg bolus, then remainder over 2 hours).
- Cardiac arrest: 50 mg bolus.
- Vasopressors
- First choice: Adrenaline or noradrenaline infusion
- Adjuncts: Vasopressin (for pressure support), dobutamine (for RV inotropy)
- Consider: adrenaline if severe refractory RV failure
- Inhaled pulmonary vasodilators
- Nitroglycerine
- Milrinone
- Nitric oxide
- Fluid-conservative therapy
Presentation
- See: Dyspnoea
- A small PE causes sudden dyspnoea, pleuritic pain and possibly haemoptysis, with few physical signs. Look for a low-grade pyrexia (>38°C), tachypnoea (>20/min), tachycardia and a pleural rub
- A major PE causes dyspnoea, chest pain and light-headedness or collapse, followed by recovery. Look for cyanosis, tachycardia, hypotension, a parasternal heave, raised JVP and a loud delayed pulmonary second sound
- Clinical signs of a DVT may be present
Red Flags
- On Examination
- Diaphoresis
- Signs of hypoperfusion: mottling, cool extremities, confusion, agitation
- Vital signs
- Bradycardia ⇒ may indicate impending brady-asystolic arrest
- Shock index (HR/SBP) > 1
- Hypotension
- Hypertension (some patients with PE have excess adrenaline production), often indicated by elevated lactate
- Tachypnoea > 30
- Labs
- Elevated troponin
- Elevated lactate
Investigations
Bedside
- Weight
Bloods
- Consider performing an ABG
- Do not routinely unless pulse oximetry is unreliable or demonstrates unexplained hypoxia on room air
- Low , Low , High pH
- Characteristic findings include acute respiratory alkalosis, or hypoxia and a raised A-a gradient
- D-dimer
- Age adjusted cutoff 0.01 x age if >50 y/o
- Coags, FBC, EUC, LFT
- beta-HCG in women of child bearing age
- Troponin (if chest pain or otherwise indicated)
ECG
- Significant PE may cause right axis deviation and right BBB but most common sign is sinus tachycardia (S1Q3T3 is neither specific nor sensitive for PE)
- Other ECG findings: Qr in V1, STE in V1, Complete RBBB, S1Q3T3, R axis deviation, STE in III, STD in V4-6, AF, TWI in precordial/inferior leads
Imaging
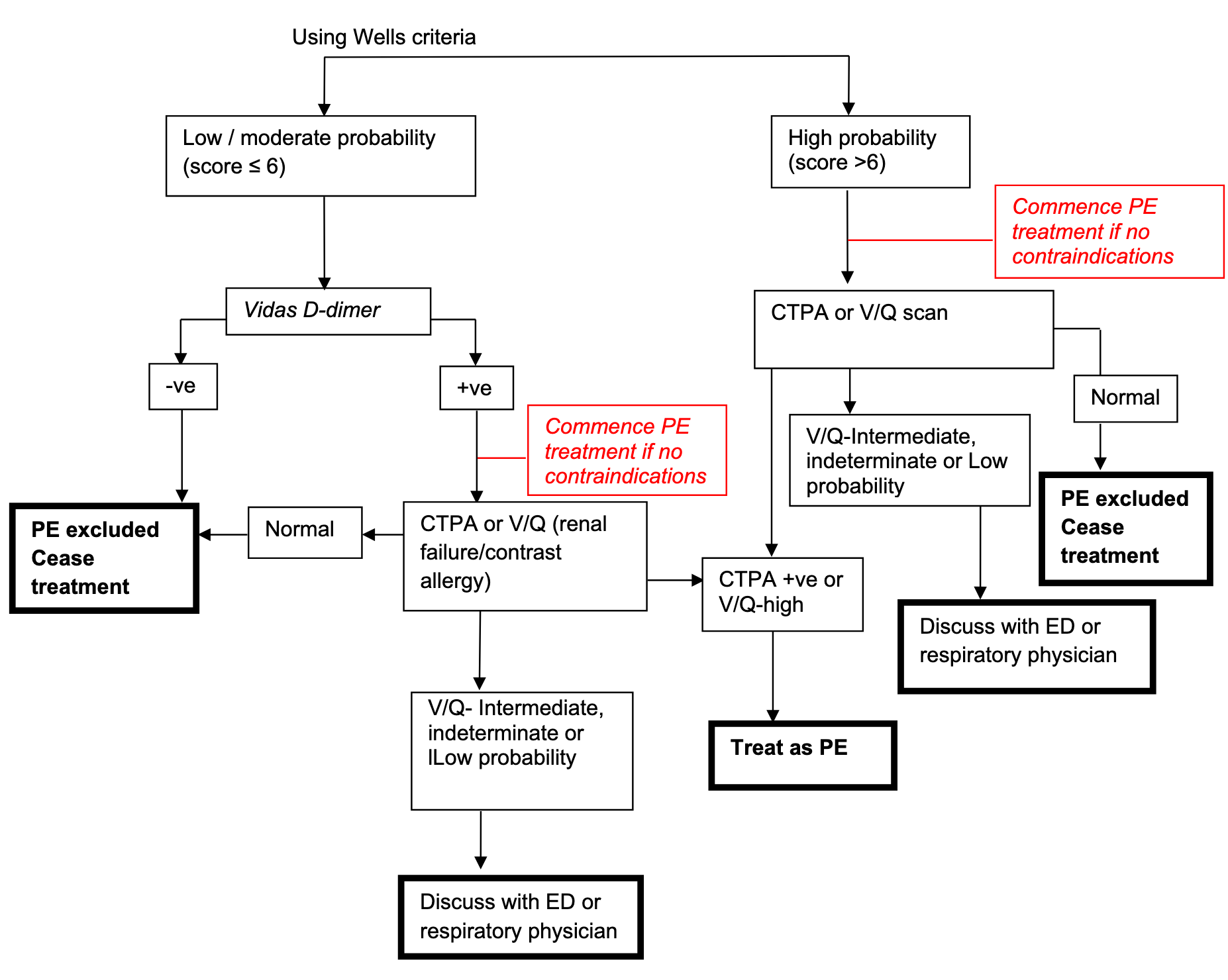
- Calculate the clinical pre-test probability of PE before requesting any diagnostic imaging

- Can use D-dimer to exclude PE in low probability pre-test patients
- Can use ELISA D-dimer to exclude PE in moderate probability pre-test patients
- If >6 proceed directly to definitive diagnostic imaging
NOTE
Only send a D-dimer test in
- Patients ≥50 years with a low pre-test probability or
- In any patient <50 with a low pre-test probability but who fails to fulfil one or more PERC criteria
- If all PERC criteria are fulfilled, the patients does not have a PE and does not need a D-dimer test sent
NOTE
Patients with high pre-test probability should be commenced on treatment if there are no contra-indications. Treatment can commence prior to definitive imaging. Consideration should be given to treating low and moderate risk patients with positive D-Dimer and no contra-indications.


- PERC needs to be 0 to rule out PE
- If PERC positive → YEARS score + D-dimer
- Arrange a CTPA or V/Q scan in:
- All patients with a high or intermediate pre-test probability
- Those with a positive D-dimer
CTPA
- CTPA has >95% sensitivity for segmental or larger PEs and ~75% for subsegmental
- CTPA is the preferred first line imaging except for patients <40 years with a normal XR chest where V/Q scan is available within hours
- Contrast-induced risks in patients with renal insufficiency can be mitigated with:
- IV pre-hydration and adequate hydration afterwards
- Witholding metformin, NSAIDs, ACE-i
- More useful if the CXR is abnormal (V/Q scan is difficult to interpret in these cases and indertiminate result more likely)
- Arrange sequential V/Q scan ±lower limb Doppler u/s or CT venogram if doubt remains
V/Q Scan
- V/Q scan preferred over CTPA if:
- Patient is allergic to contrast dye
- Patient has renal failure
- When the CXR is normal
- Younger females
- A normal V/Q scan rules out clinically important PE in patients with low-to-moderate pre-test probability
- Interpretation of results
- Normal Scan = No PE. Consider alternate diagnosis
- Low Probability Scan + Low PTP = No PE. Consider alternate diagnosis
- Low Probability Scan + Intermediate or High PTP = Inconclusive result – Further testing (CTPA) required
- Intermediate Probability Scan = Inconclusive result – Further testing (CTPA) required
- High Probability Scan = PE. Commence treatment.
Chest-Xray
- Frequently normal; mainly to exclude other diagnoses such as pneumonia or pneumothorax
- Plate or linear atelactasis
- Unilateral pleural based wedge shaped pulmonary infiltrate
- Unilateral pleural effusion
- Raised hemidiaphragm
- Dilated pulmonary artery in massive PE
- Areas of oligaemia in massive PE
Pregnancy
- D-dimer cannot be used for risk stratification in pregnant patients
- Bilateral lower limb ultrasound remains the first test of choice
- In suspected PE in pregnancy, if compression ultrasonography of the legs is normal and a XR chest has not further aided the diagnostic process, the decision then needed is whether to investigate further with CTPA or V/Q or treat empirically
Risks
- The average human receives about 3mSv of “background” radiation per year. In general, the comparative radiation dose to a patient with CTPA is 12 mSv whilst it is 2.3mSv with V/Q scan.
- The natural background dose for a foetus during pregnancy is 1.1-2.5mGy. The foetal dose of radiation from CTPA is 0.37mGy, whilst it is 0.4mGy from a V/Q scan in early pregnancy and 0.75mGy at 6 months. The risk of childhood cancer in exposed offspring is slightly higher with V/Q scan than with CTPA (1 in 280,000 for V/Q and %3C1 in 1,000,000 for CTPA)
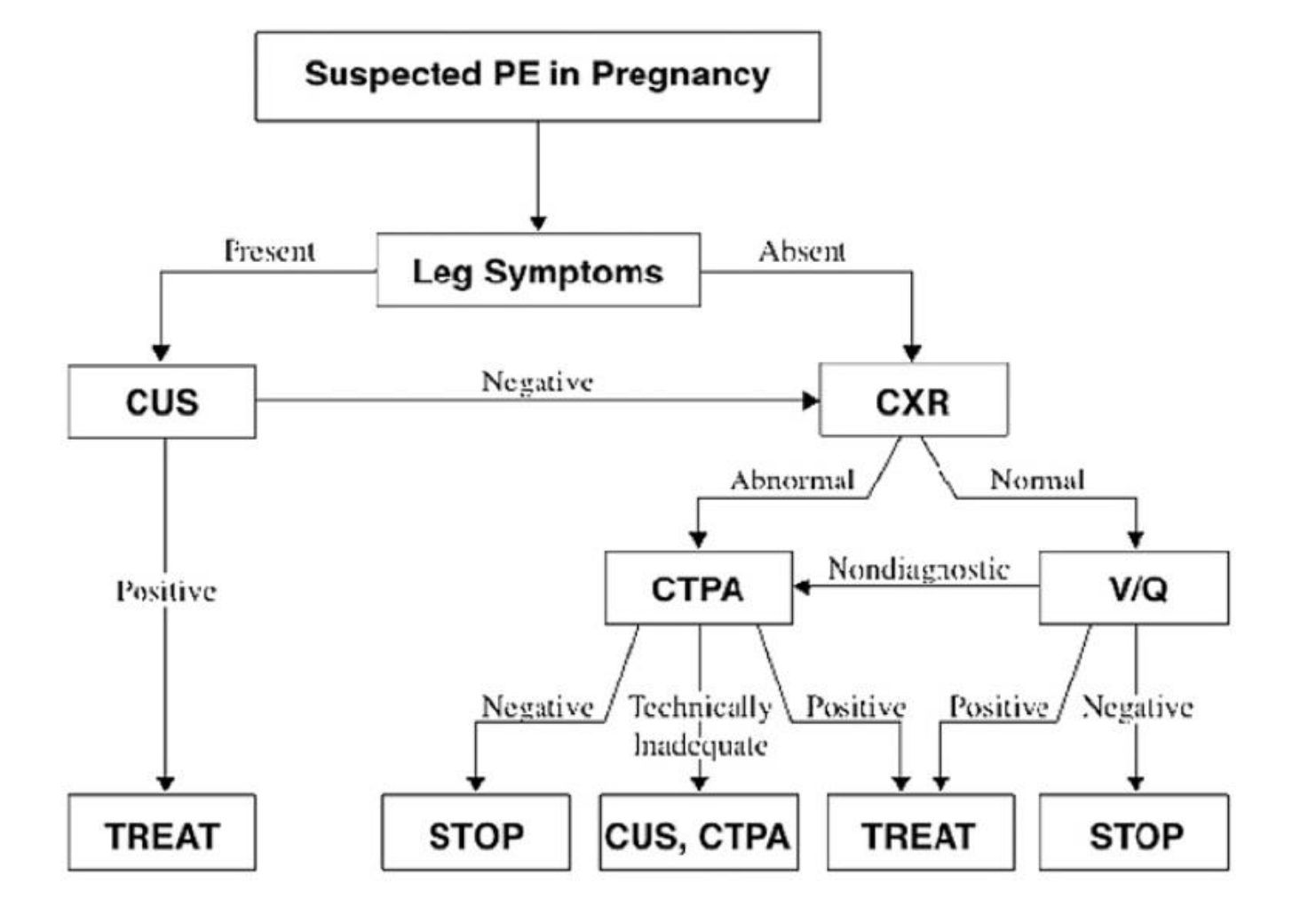
- CUS = Lower limb ultrasound
Management
General measures
- Give high-dose oxygen, aiming for oxygen saturation >95%
- Lie patient flat to increase venous return
- Give IV normal saline to support BP if necessary (can trial 250mL normal saline bolus)
- **Avoid excessive fluid ∵ worsens RV dilation → septal shift → worsens LV function **
- Patients who are really unwell from massive PE have elevated filling pressures, the potential risk of fluid generally outweighs the potential benefit in these patients
- Vasopressors: Norad first line, dobutamine
- Relieve pain with titrated morphine 2.5 mg IV boluses
- Can use PESI score or simplified PESI score to determine risk of 30 day mortality (see here)
- Measure weight and creatinine clearance before selecting anticoaglant
- See contraindications to thrombolysis and anticoagulation here
Anticoagulation
- Commence anticoagulation when:
- The diagnosis is confirmed or
- When there is an intermediate or high pre-test probability of PE but a delay to testing (in the absence of contraindications)
- 2 anticoagulation options exist:
- Heparin: UFH or LMWH
- NOAC
- Duration
- Provoked: minimum 3 months
- Unprovoked: >3 months
- Cancer associated: >6 months
- Can use DOAC or clexane
- LMWH for GI/GI cancers and high bleeding risk
- DOAC can be used for lung, breast, prostate, haem (unless thrombocytopenia), ovarian, brain
- Can use DOAC or clexane
Heparin + Warfarin
- Give LMWH such as enoxaparin 1mg/kg SC BD
- LMWH does not require aPTT monitoring
- In patients with haemodynamic compromise, give UFH (80 U/kg IV bolus) followed by maintenance infusion of 18 U/kg/h titrated to aPTT (1.5-2.5x control value)
- If patient already on warfarin and has a PE consult cardiothoracics for consideration of transvenous vena caval filter
- Commence first dose of warfarin 5mg PO on the first day of heparin therapy and titrate ssubsequent daily doses to achieve an INR of 2.5-3.5
NOAC/DOAC
- NOAC such as rivaroxaban 15mg PO 12 hourly or apixabanm 10mg PO 12-hourly
- Check renal function
- Cannot use in child-pugh class B or worse without specialist input
Dabigatran
Dabigatran requires at least 5 days of parenteral anticoagulant to be given first. Dose is 150mg PO 12-hourly. Dose modification is required based of renal function
Massive PE
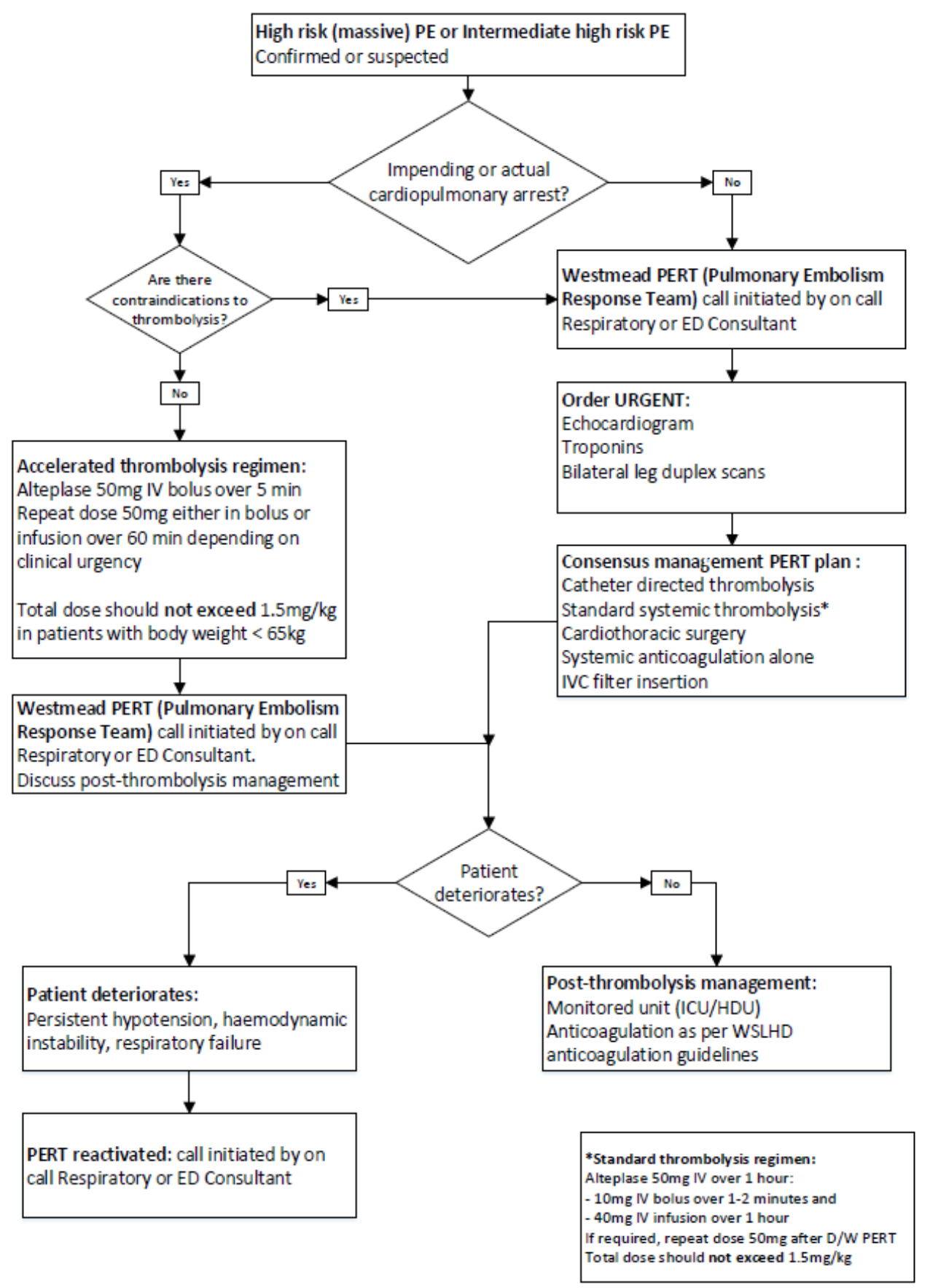
- Consider when the probability of PE is high (or confirmed) and:
- The patient is hypotensive despite fluid resuscitation and/or
- Has evidence of acute RV failure and/or
- Is peri-arrest
- High risk (previously massive) PE:
- Acute PE (confirmed on VQ, CTPA or bedside echocardiogram) accompanied by any of:
- Sustained hypotension (systolic BP <90 mmHg for at least 15 min or requiring ionotropic support not due to a cause other than PE)
- Pulselessness
- Persistent profound bradycardia (heart rate <40 bpm with symptoms or signs of shock)
- Acute PE (confirmed on VQ, CTPA or bedside echocardiogram) accompanied by any of:
- Intermediate high risk (previously sub-massive) PE:
- Acute PE without systemic hypotension (systolic BP >90 mmHg) but with either right ventricular dysfunction and/or myocardial necrosis:
- RV dysfunction defined as at least one of:
- RV dilation (apical 4-chamber RV diameter divided by LV diameter ≥0.9) or RV systolic dysfunction on echocardiography
- RV dilation (4 chamber RV diameter divided by LV diameter ≥0.9) on CT
- Elevation of BNP (>90 pg/mL) or pro BNP (>500 pg/mL)
- ECG changes indicating RV dysfunction (new RBBB, anteroseptal ST elevation or depression or T wave inversion)
- Myocardial necrosis defined by:
- Elevation of troponin T >50ng/L
- RV dysfunction defined as at least one of:
- Acute PE without systemic hypotension (systolic BP >90 mmHg) but with either right ventricular dysfunction and/or myocardial necrosis:
- Call immediate senior help and MET Activation Criteria
- Stat fibrinolytic doses can be given in cases of cardiac arrest considered related to a massive PE
- Catheter directed thrombolysis indicated for patients with acute PE associated with hypotension who have:
- High bleeding risk
- Failed systemic thrombolysis
- Shock that is likely to cause death before systemic thrombolysis can take effect (e.g. within hours)
Other Management in Massive PE
Avoid Intubation
- Avoid intubation unless the patient has lost mental status or has developed respiratory exhaustion as it often precipitates cardiac arrest because:
- Sedatives drop blood pressure
- Positive pressure reduces preload
- Over-distention of the lungs may compress pulmonary capillaries, increasing the pulmonary vascular resistance
- Avoid intubation by:
- High flow nasal cannulas combined with pulmonary vasodilators
- Give thrombolysis first (if indicated) then intubate later
- Optimising for intubation:
- Increase SBP to 130-140 with adrenaline/noradrenaline infusion
- Use sedatives that are haemodynamically stable (e.g. ketamine)
- Following intubation, don’t over-distend the lungs (i.e. avoid over-vigorous bag ventilation)
Careful Administration of Fluids
- Evaluate with ultrasound
- If clear evidence of hypovolaemia (e.g. small IVC with variation with respiration), give fluid in small amounts
- Small IVC rarely occurs in massive PE; if seen should consider alternative diagnoses to massive PE
- If IVC dilated do not give fluid
- If already received fluid consider diuresis
Inotropes and Vasopressors
- Noradrenaline
- Establishing an adequate mean arterial pressure (e.g. >65 mm) will help ensure adequate perfusion of the right coronary artery and thereby support right ventricular function
- See Inotropes
Inhaled Pulmonary Vasodilators
Sources
- On Call: Principles and Protocols
- Derranged physiology: https://derangedphysiology.com/main/required-reading/respiratory-intensive-care/Chapter-161/pulmonary-embolism
- IBCC: Submassive & Massive PE https://emcrit.org/ibcc/pe/
- Local hospital guidelines (NSW)
- ACI guidelines: https://aci.health.nsw.gov.au/networks/eci/clinical/tools/respiratory/pe