Priorities in Assessment
- Obtain 12-Lead ECG
- Condition of the patient (presence or absence of adverse features):
- Remember as: compromise of circulation - systemic, cerebral, pulmonary or cardiac
- Shock - hypotension (SBP < 90mmHg), pallor, sweating, cold extremities, confusion or impaired consciousness
- Syncope
- Heart failure - pulmonary oedema and/or raised jugular venous pressure
- Myocardial ischaemia - typical ischaemic chest pain and/or other evidence of myocardial ischaemia on a 12-lead ECG
- Heart rate
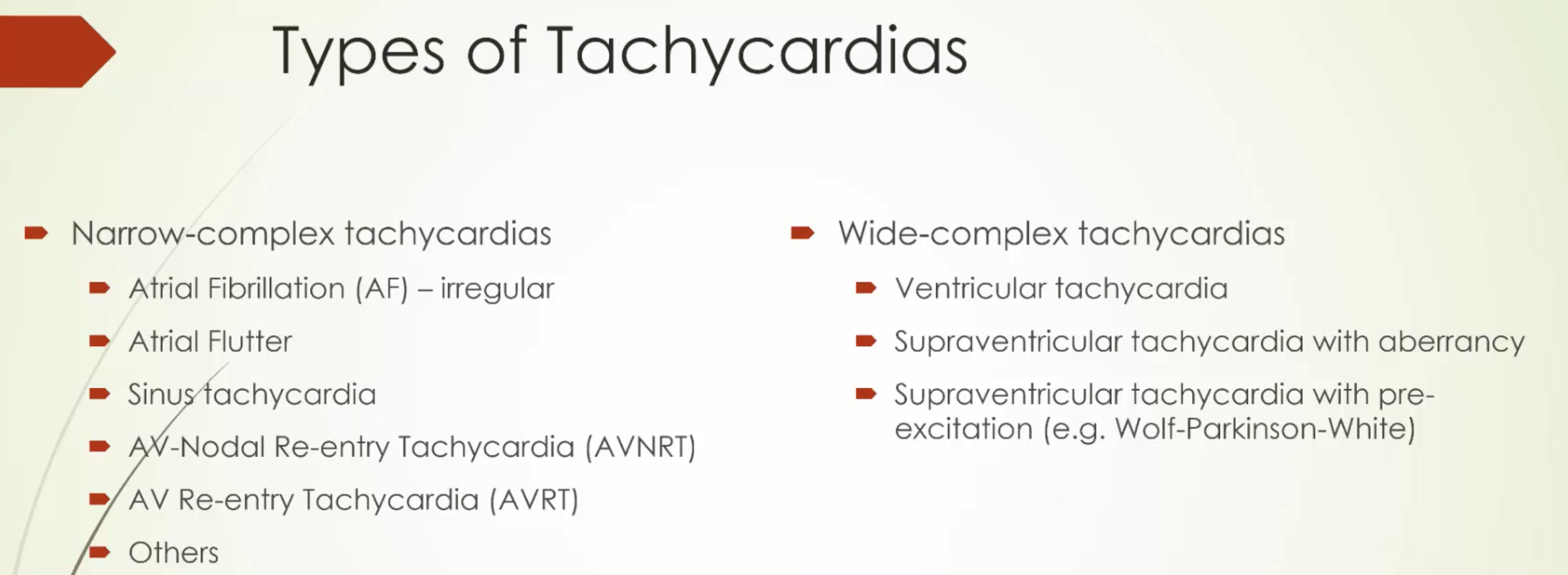
Tachyarrhythmias
Phone Call/Presentation Questions
- Heart rate?
- Regular or irregular?
- Blood pressure?
- Chest pain, dyspnoea or altered mental status?
- History of illicit durg use?
- Temperature?
- Reason for admission?
Instructions over the phone
- When the patient has chest pain, SOB, SBP <90mmHg or altered mental status:
- Ask the nurse to stay by the patient’s bedside and get help from additional nursing staff
- Give oxygen by mask to maintain saturation >94% and attach monitoring (pulse oximeter and cardiac monitor, request an ECG)
- Request IV trolley for patient’s bedside with two cannulae ready for insertion
- Request the cardiac arrest trolley with defibrillator and resuscitation equipment be brought to the patient’s bedside
- See any patient with tachycardia and signs of circulatory compromise such as chest pain, SOB, hypotension or an altered mental status immediately; or if the HR >140 beats/min, as this will trigger a MET call
Common Causes
NOTE
AVNRT is the most common cause of palpitations in patients with structurally normal hearts
- Rapid regular heart rate
- Sinus tachycardia
- Atrial flutter (with constant AV conduction 2:1 or 3:1)
- Supraventricular tachycardia
- Paroxysmal atrial tachycardia
- Junctional tachycardia
- Ventricular tachycardia
- Rapid irregular heart rate
- Atrial fibrillation with rapid ventricular response
- Atrial flutter with variable AV conduction/block
- Multifocal atrial tachycardia
- Sinus tachycardia with PACs or PVCs
Assessment
End of Bed
Patients who are normotensive with a tachycardia or arrhythmia may look deceptively well
A → E Assessment
- Heart rate
- Take the patient’s pulse, listen to the apex beat or read the ECG rhythm strip
- Feel for the volume of the pulse and its regularity
- ECG
- Does the ECG also demonstrate ischaemic changes?
- Steps in assessing a tachycardia in an ECG:
- Wide vs narrow complex (narrow = SVT, wide = VT)
- Regular vs irregular
- P waves and origin
- Broad-complex tachycardia in an older patient, or in any patient with known prior myocardial ischaemia, is probably VT and should be treated as such
- Blood pressure
- If hypotensive can be due to:
- Hypotension with a compensatory tachycardia (usually sinus, but may be AF)
- Tachycardia causing hypotension (most commonly VT, AF with RVR and SVT)
- If hypotensive can be due to:
- Respiratory rate
- Consider if the patient has APO
Immediate Management
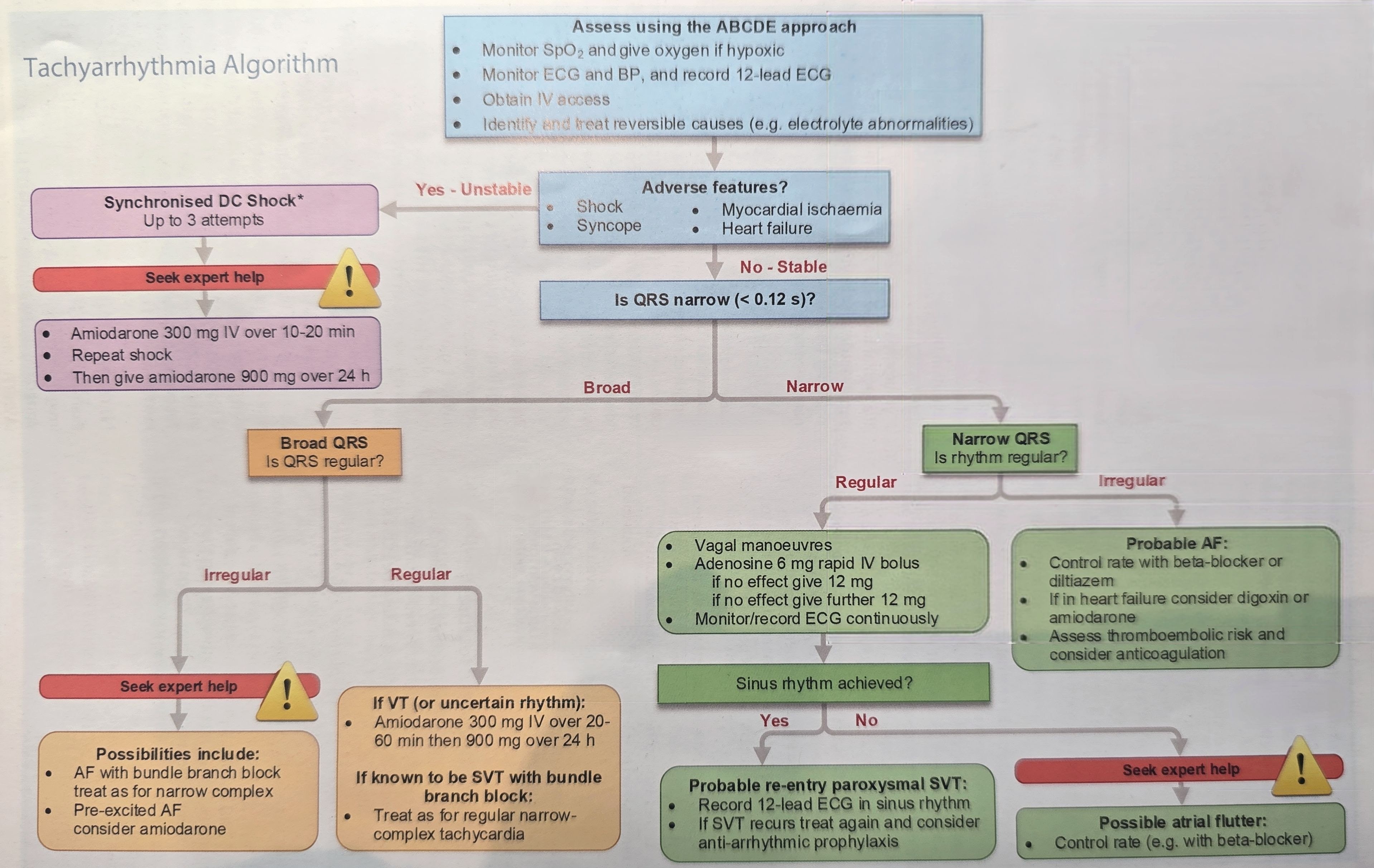
- Narrow complex tachycardia without a pulse
- If the patient is pulseless with a rapid narrow complex tachycardia they have PEA and you should start CPR
- Arrange immediate syncrhonised cardioversion at 200J as soon as possible
- If synchronised is not possible deliver DC shock as in ALS
- Tachycardia in a haemodynamically unstable patient with hypotension, chest pain, SOB and/or altered mental status:
- Call for senior help
- Apply high-flow oxygen by mask, and gain IV access
- Attach an ECG monitor/defibrillator to the patient
- Confirm the cardiac rhythm with a 12-lead ECG (do not try to diagnose the rhythm without a formal 12-lead ECG, except in a dire emergency)
- Prepare procedural sedation, such as propofol 200 mg in 20 mL IV, and keep readily available. Call an anaesthetist, as cardioversion will be required
- A patient who is haemodynamically unstable and has VT, AF with rapid ventricular response or SVT requires emergency synchronised DC cardioversion
- Unless the patient is in cardiac arrest (in which case an immediate non-synchronised shock is given), always wait for senior staff to attend. Never administer procedural sedation and proceed to electrical DC cardioversion alone
- One doctor must attend to the airway, while the other operates the defibrillator and coordinates the cardiac care
- Must be synchronised so that the shock is triggered by the R wave on the ECG (anticipate a slight delay); if synchronisation fails, choose another lead and/or adjust the amplitude
- Broad-complex tachycardia or atrial fibrillation: Start with 120–150 J biphasic and repeat up to three times, with stepwise increases in joules
- Atrial flutter and regular narrow-complex tachycardia: start with 70-120 J
- For atrial fibrillation and flutter use anteroposterior defibrillator pad positions
- When delivering the shock, press the shock button and retain the pressure to keep it pressed until after the shock has occurred - there may be a slight delay before the shock is delivered
- If a second or third shock is needed, reactivate the synchronisation switch if necessary
- If cardioversion fails and adverse features persist, give amiodarone 300mg IV over 10-20 minutes and attempt further synchronised cardioversion; consider starting at the same energy level as the previous attempt
- The loading dose of amiodarone can be followed by an infusion of 900 mg over 24 hours given into a large vein (preferably central access)
- Note: if the patient is hypotensive and the rhythm is sinus tachycardia, the most likely cause is underlying hypotension.
- Look for and urgently treat any cause(s) for this, such as hypovolaemia, hypoxia, fever etc, and consider other precipitants of the tachycardia, such as anaemia or pain
- Haemodynamically stable patient with broad complex tachycardia may be VT or SVT with bundle branch block
- Treat with amiodarone 300mg IV over 20-60 minutes, followed by an infusion of 900 mg over 24h
- If a regular broad complex tachycardia is known to be a supraventricular arrhythmia with a bundle branch block and the patient is stable, treat as a narrow-complex tachycardia
Selective History and Chart Review
- Only if the patient is stable or immediate management has been commenced and help is on its way
- Onset of palpitations?
- Sudden onset ⇒ new acute arrhythmia
- Gradual onset ⇒ worsening of chronic arrhythmia such as AF
- Recurrent intermittent episodes ⇒ paroxysmal arrhythmia or ectopic beats
- Following chest pain ⇒ ischaemia as the cause; palpitations followed by pain ⇒ ischaemia 2° to arrhythmia
- Related symptoms?
- Sweating, light-headedness, chest pain, dyspnoea or syncope ⇒ circulatory compromise
- PMHx
- Patient’s cardiac history?
- Previous episodes, investigations, treatment given and success (e.g. patients with SVT may have had vagal manoeuvre or adenosine)
- Precipitating factors:
- Chest pain, dizzy spell or collapse
- Ischaemic heart disease, atherosclerosis risk factors (SNAPW, hypertension, hypercholesterolaemia, diabetes, renal disease, positive family history)
- Pericarditis
- Structural heart disease (e.g. valvular disease, cardiomyopathy, congenital heart disease or recent cardiac surgery)
- Thyroid disease
- Illicit drug use such as cocaine or amphetamines
- Family history of palpitations, syncope or sudden cardiac death?
- Premature sudden death consider WPW, Brugada syndrome, long QT syndrome or HCM
- Patient’s cardiac history?
- Charts
- Previous ECGs
- Medications causing tachycardias (e.g. salbutamol, terbutaline, pseudoephedrine or anticholinergics)
- Previous echocardiography reports
Examinations
| Examination | Notes |
|---|---|
| Vitals | Repeat |
| HEENT | Exopthalmos, lid lag, lid retraction ⇒ hyperthyroidism |
| CVS | Murmurs of mitral regurgitation or mitral stenosis ⇒ mitral valve disease |
| S3 gallop ⇒ LV failure | |
| Resp | Tachypnoea, cyanosis, wheezing, pleural effusion ⇒ LV failure, PE |
| MSS | Swelling, thigh or leg tenderness or oedema ⇒ DVT |
| Tremor, brisk deep tendon reflexes ⇒ hyperthyroidism |
Treatment of Regular Narrow-Complex Tachyarrhythmia
- Start with vagal manoeuvres
- Record an ECG (preferably 12-lead during each manoeuvre). If the rhythm is Atrial Flutter with 2:1 conduction, transient slowing of the ventricular response will often occur and reveal flutter waves
- If the arrhythmia persists and is not atrial flutter, give adenosine 6mg as a very rapid IV bolus followed by a flush ⇒ use a relatively large cannula and a large vein
- Use a three way tap with pressure bag infusion with one port for the adenosine and the other for the flush
- Warn the patient that they will feel unwell, chest discomfort or near blackout like feeling for a few seconds
- Record a 12-lead ECG during the injection and observe if the ventricular rate slows transiently, but then speeds up again, look for atrial activity, such as atrial flutter or other atrial tachycardia and treat accordingly
- If no response (i.e. no transient slowing or termination of the tachyarrhythmia) give a 12mg bolus. If there is no response give one further 12mg bolus. Also consider if the bolus is given too slowly or into a peripheral vein
- If adenosine is contraindicated consider given verapamil 2.5-5mg (avoid in patients with cardiac failure, hypotension, concomitant ß-blocker therapy or WPW) or metaraminol 1mg1
Treatment of Irregular Narrow-Complex Tachyarrhthmia
- Most likely AF with rapid ventricular response
- If presence of adverse features, perform synchronised cardioversion, otherwise start anticoagulation prior to cardioversion initially with LMWH or UFH at the earliest opportunity
- Treatment options include:
- Rate control by drug therapy: metoprolol, particularly for IV use (1mg IV aliquots up to 5mg to response) or diltiazem in patients in whom beta-blockade is contraindicated or not tolerated. Digoxin my be used in patients with heart failure (but not if already on amiodarone)
- Rhythm control using drugs to achieve chemical cardioversion
- Rhythm control by synchronised cardioversion
- Treatment to prevent complications
- In general, patients in AF>48h should not be treated by cardioversion until they have been fully anticoagulated, and/or unless TOE has detected no evidence of atrial thrombus
Specific Management
- Atrial fibrillation (management is also similar for atrial flutter)
- SVT
- Ectopic atrial tachycardias and junctional tachycardias for the most part I’m not sure; ask a cardiologist
- Sinus tachycardia: treat the underlying cause; most common causes include
- Hypovolaemia, hypoxia of any cause, LV failure, fever or infection, hyperthyroidism, anaemia, sympathomimetic or anticholinergic drugs, pain or anxiety
- Sinus tachycardia with PVCs
- Assess for malignant features:
- R on T phenomenon
- Multifocal PVCs
- Couplets or salvos with three or more PVCs in a row (non-sustained VT)
- Frequent PVCs (>5/min)
- Assess for underlying cause e.g.
- Hypoxia
- Myocardial ischaemia
- Hypokalaemia
- Acid-base imbalance
- Cardiomyopathy and MVP
- Drugs such as digoxin and other antiarrhythmic agents
- Hyperthyroidism
- Transfer the patient to a telemetry ward or CCU for further investigation and continuous ECG monitoring
- Assess for malignant features:
- Ventricular Tachycardia
Bradyarrhythmias
Phone Call/Presentation Questions
- Heart rate?
- Blood pressure?
- Is the patient on digoxin, beta-blocker, calcium channel blocker or other antiarrhythmic drug?
- Reason for admission
Instructions over the phone
- When the patient has HR <40, SBP <90mmHg or features of circulatory compromise
- Oxygen by mask to maintain saturation >94% and attach pulse oximeter and cardiac monitoring to the patient
- Consider asking the nurse to temporarily place the patient in Trendelenburg position if the patient is hypotensive but beneficial effect is transitory and may result in raised intracranial pressure and aspiration
- Request an urgent 12-lead ECG
- Ask for an IV trolley at the patient’s bedside, with two cannulae, ready for your arrival
- Request the cardiac arrest trolley with defibrillator, pacer and resuscitation equipment to be brought to the patient’s bedside and atropine 1mg drawn up ready
- See any patient with a bradycardia and signs of circulatory compromise such as chest pain, SOB, hypotension or an altered mental status immediately; or if the HR <40 beats/min, as this will trigger a MET call
Common Causes
- Bradyarrhythmias include
- Sinus bradycardia
- Junctional bradycardia
- First degree AV block
- Second degree AV block
- Type 1 (Wenckebach): ↑ PR interval untl beat dropped
- Type 2: Normal or short PR interval with dropped beat
- Third degree AV block
- AF with a slow ventricular rate
- Causes of bradyarrhythmias include
- Drugs: antiarrhthymic agents (beta blockers, calcium channel blockers, digoxin, amiodarone, sotalol)
- Cardiac disease: Acute MI (esp. inferior wall) sick sinus syndrome
- Other: Vasovagal attack, healthy young athletes, hypothermia, hypothyroidsim, increased ICP in association with hypertension (Cushing’s reflex)
Assessment
Link to original
- Heart rate
End of Bed
- If concerned tell the nurse to bring the cardiac arrest trolley to the bedside and attach an ECG monitor to the patient; consider MET call
A → E Assessment
- Heart rate?
- Read the ECG or palpate the patient’s pulse to identify the rate
- Heart rhythm?
- ECG
- Look for any association between P waves and the QRS complexes; determine if sinus bradycardia or AV block
- Consider junctional bradycardia if rhythm regular but no P waves or slow AF if it is regular with no P waves
- Blood pressure?
- Most causes of hypotension are accompanied by reflex tachycardia however 5-10% of haemorrhagic shock can have bradycardia
- Otherwise, bradyarrhythmia is likely to be responsible for hypotension
- Temperature?
- Hypothermia may be associated with bradyarrhythmia
Immediate Management
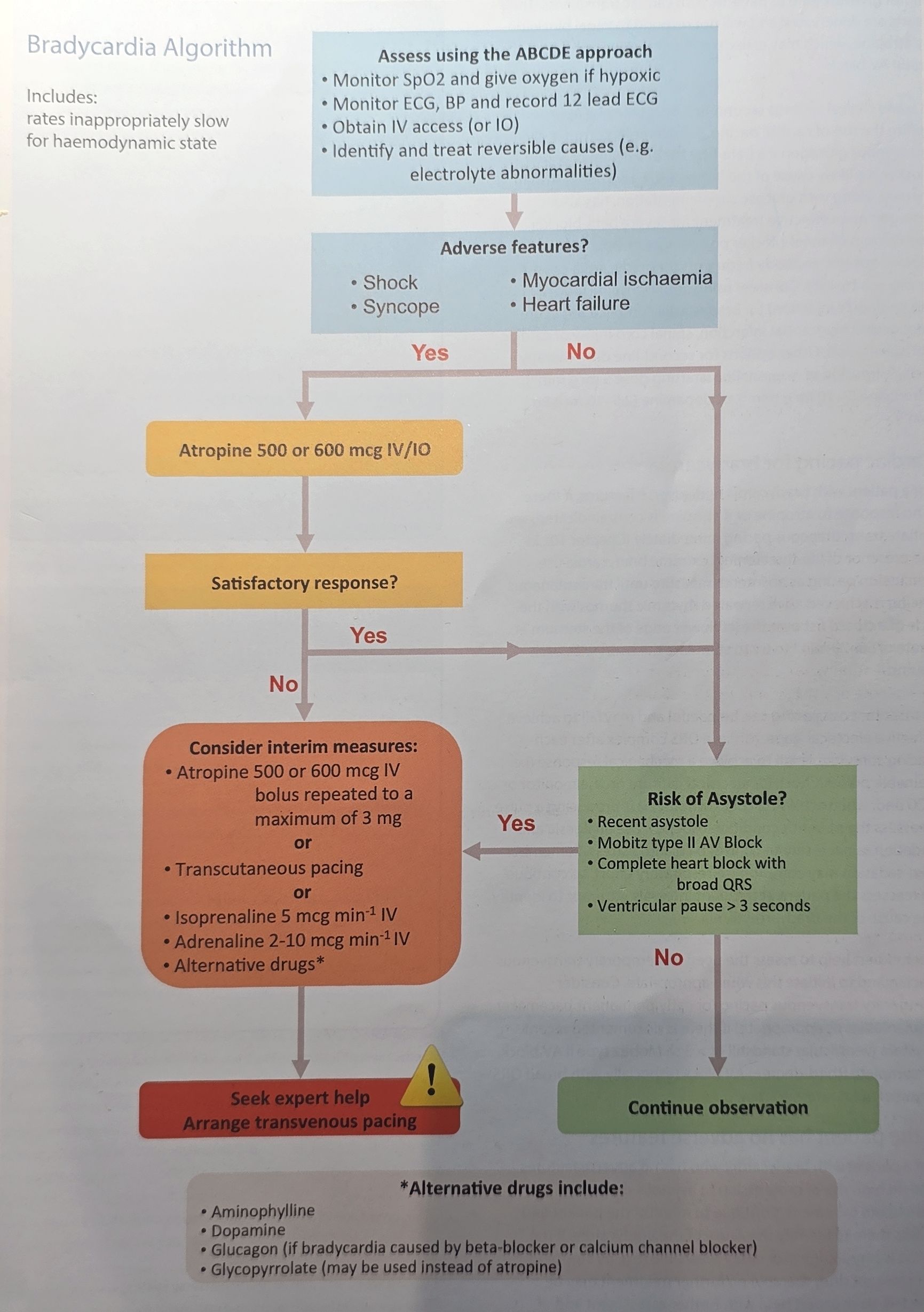
- If adverse features:
- Call senior for help
- Apply high-flow oxygen by mask and gain IV access
- Attach an ECG monitor/defibrillator to the patient and confirm rhythm
- Elevate patient’s legs temporarily in the Trendelenburg position
- Give atropine 500mcg IV rapid bolus and if necessary repeat every 3-5 minutes to a total of 3mg (doses of atropine given slowly or of <500mcg can cause paradoxical slowing of the heart rate
- Use atropine cautiously in the presence of acute myocardial ischaemia or myocardial infarction
- Do not give atropine to patients with cardiac transplants
- If bradycardia with adverse signs persists: consider cardiac pacing, otherwise consider second line drugs
- Transcutaneous pacing:
- Organise transthoracic pacing if still no improvement and the patient is symptomatic (requires small amounts of midazolam 1.25-2.5mg or diazepam 2.5mg IV as the procedure is uncomfortable); consider second line as well as analgesia (e.g. fentanyl)
- While organising pacing, use percussion pacing as an interim measure: repeated rhythmic thumps with the side of a closed fist over the left lower edge of the sternum at a rate of 50-70 beats/min
- Remember to attach limb leads to the pacing defibrillator
- Turn on asyncronous pacing using the buttons on the bottom of the defibrillator (bottom right)
- Set rate using the rate dial (70 bpm)
- Set the power output using mA dial (patients usually require 60-70 mA)
- Obtain capture: (downward pacing spike followed by a QRS complex and T wave)
- Set power output to 10% above the threshold
- Check mechanical capture by checking pulse and blood pressure
When to Give other Drugs instead of Atropine
- Glucagon if a beta block or calcium channel blocker is likely cause of bradycardia
- High dose insulin therapy along with glucose supplementation can also work
- Digoxin-specific antibody fragments for bradycardia caused by digoxin toxicity
- Aminophylline (100-200 mg) by slow IV injection for bradycardia complicating acute inferior wall myocardial infarction, spinal cord injury or cardiac transplantation
Selective History and Chart Review
- Previous episodes of bradycardia or heart block?
- Cardiac risk factors (e.g. smoking, hypertension, hypercholesterolaemia, diabetes, renal impairment)
- History of angina or previous acute MI
- Recent symptoms suggestive of an ischaemic event (e.g. chest pain, nausea or vomiting)
- Charts
- Medication chart: drugs that might cause bradycardia including antiarrhythmic agents (e.g. beta blockers, calcium channel blockers, digoxin, anmiodarone or sotalol)
Examinations
| Examinations | Notes |
|---|---|
| Vitals | Bradypnoea ⇒ hypothermia, hypothyroidism |
| Hypothermia ⇒ hypothyroidism | |
| Hypertension ⇒ underlying CAD | |
| HEENT | Coarse facial features ⇒ hypothyroidism |
| Loss of lateral third of eyebrows ⇒ hypothyroidism | |
| Periorbital xanthomas ⇒ CAD | |
| Fundi with hypertensive or diabetic changes ⇒ CAD | |
| CVS | Mitral regurgitant murmur ⇒ recent acute MI |
| GIT | Renal, aortic or femoral bruits ⇒ CAD and atherosclerosis |
| Neuro | Delayed return phase of deep tendon reflexes ⇒ hypothyroidism |
Specific Management
- Sinus bradycardia
- No immediate treatment is required if the patient is not hypotensive
- If the patient is on digoxin with a HR <60 beats/min, withhold further digoxin until the HR is >60 beats/min
- If the patient is on medication that depresses conduction, withhold the next dose until the HR is >60 beats/min
- Atrial Fibrillation
- AV block 2nd and third degree will need temporary pacing while addressing reversible causes or permanent pacemaker
Footnotes
-
Have personally seen this, in a patient who did not want adenosine, although as with everything on this website not formal medical advice. Also see: https://litfl.com/im-so-old-that/ ↩