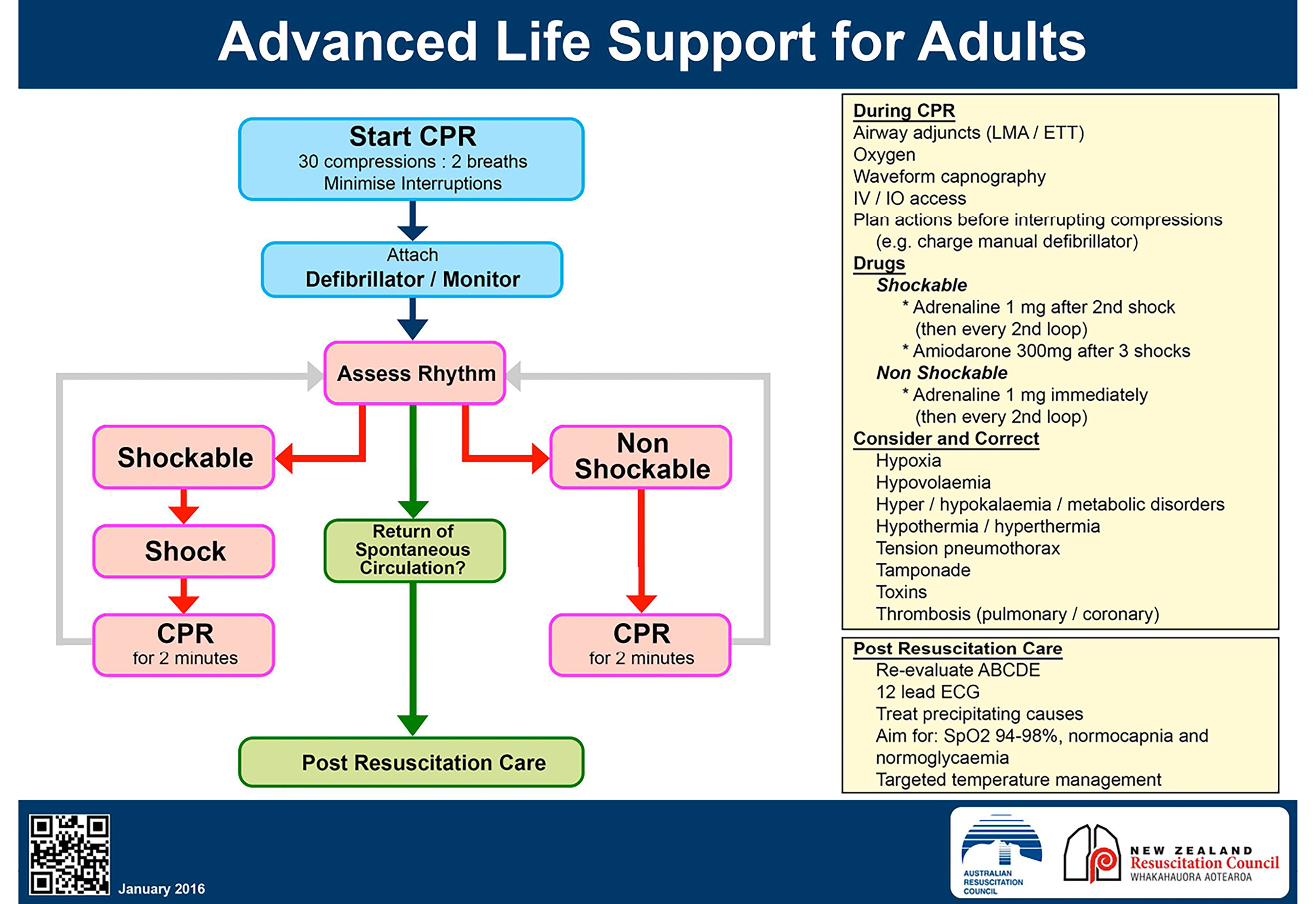
ALS Algorithm
NOTE
The highest priorities in resuscitation is:
- Good quality CPR
- Ensuring help is on the way
- Reducing time to defibrillation Once defibrillator pads are attached, do a rhythm assessment as soon as possible. Chest compressions and ventilation must be undertaken immediately but should not delay attempts to deliver the first shock to defibrillate those patients in VF/pVT
- Defibrillator attachment and usage
- Right of the sternum below the clavicle and mid-axillary line at 5th or 6th intercostal space
- Do not defibrillate over ECG electrodes or leads, GTN patch, internal devices such as a pacemaker or jewellery
- Shave off excessive hair; however in very hairy patients, a bi-axillary electrode position enable more rapid defibrillation
- Although they are marked positive and negative, each can be placed in either position
- Other acceptable positions:
- One electrode anteriorly, over the left precordium, and the other electrode on the back behind the heart, just inferior to the left scapula (preferred position for transcutaneous pacing)
- Each electrode on the lateral chest walls, one on the right and the other on the left side (bi-axillary)
- One electrode placed in the mid-axillary line, approximately level with the V6 electrode and the other electrode on the back, just inferior to the right scapula (postero-lateral)
- In patients with an ICD, place the electrode at least 10cm (if possible 15cm) away or use an alternative electrode position
Monitored and Witnessed Cardiac Arrest
If a patient has all of the following:
- Monitored and witnessed cardiac arrest
- Immediately prior to the arrest was well oxygenated and perfused
- A manual defibrillator is rapidly available or the patient is already connected to the defibrillator
- It is possible to deliver the first shock within 20 seconds of the arrest onset
Then:
- Confirm cardiac arrest and shout for help
- Give three quick successive (stacked) shocks
- Rapidly check for rhythm change and, if appropriate check for a pulse and other signs of ROSC after each defibrillation attempt
- Start CPR if the third shock is unsuccessful
- If unsuccessful continue with ALS algorithm with these ‘stacked’ shocks count as the first defibrillation attempt
Rhythm Assessment
- Classified into 3 groups:
- Shockable rhythyms (VF, pVT)
- Asystole
- PEA
Shockable Rhythms
- The only two shockable rhythms are1:
- Ventricular fibrillation2 ⇒ check the patient immediately to establish whether the appearance is due to artefact; if the patient is conscious or has a pulse, the rhythm is not VF
- Pulseless ventricular tachycardia
- Do not delay defibrillation for any other procedure
- First shock (200J biphasic or 360J monophasic)
- If cardiac arrest is witnessed and monitored with a defibrillator immediately available give one shock
- In a witnessed and monitored ventricular fibrillation arrest, three stacked shocks are indicated if able to be commenced within 20 seconds
- Immediately commence CPR 30:2 for 2 minutes
- Establish IV/IO access whilst CPR in progress
- At the end of two minutes CPR, state prepare to defibrillate and apply COACHED
COACHED Approach
- Continue compressions
- Oxygen away (≥1m away)
- All others away (visual check)
- Charging (top, middle bottom clear)
- Hands off (request CPR to say “I am safe” or “pause compressions” if mechanical CPR)
- Evaluate rhythym (±pulse check)
- Defibrillate (delivering shock) or Dump charge
- Recommence CPR immediately after shock delivery: state loudly: Recommence CPR
- Do not check for rhythm or pulse and just recommence CPR immediately3
- Reassess patient and monitor rhythm after one cycle (five sets of 30 compressions:2 breaths over 2 minutes); remember to state prepare to defibrillate and apply coached mnemonic above
- Repeat a single shock (200J biphasic or 360J monophasic) if there is persistent VF or pVT, consider increasing to 360J for the second shock
- Obtain IV access and administer adrenaline 1 mg IV after the second shock
- Continue the reassess-defibrillate-CPR cycle
- Give amiodarone 300 mg IV diluted in 5% dextrose up to 20 mL after the third shock
- Repeat adrenaline 1 mg IV after the fourth shock and every two cycles thereafter (approximately 4 minutes)
- An additional dose of amiodarone 150 mg IV can be considered
- Minimuse interruptions to CPR:
- LMA insertion should be attempted without interrupting CPR
- ETT intubation should take no more than 5-10 seconds
- Can consider cricoid pressure while intubating (this is the application of pressure to the cricoid cartilage with the thumb and first fingers in the posterior direction; only remove the pressure when instructed by the person performing intubation which is usually only when the endotracheal tube is inflated)
- Reassess the patient and rhythm every 2 minutes
- In a few cases of patients who are in VF, they are difficult to cardiovert (i.e. either remain in VF or keep developing recurrent VF), consider a change in electrode position (see defibrillator position)
Organised Electrical Activity Present
- If at the 2-minute reassessment organised electrical activity is present, dump the charge of the defibrillator and feel for a pulse:
- If no pulse, continue CPR but switch to the non-shockable algorithm
- If a pulse is present, commence post-resuscitation care
Non-Shockable Rhythms
-
Non shockable rhythms is basically anything not shockable:
- Asystole
- Pulseless electrical activity4
-
Dump the charge
-
Check patient for ROSC
-
Asystole: Check that the leads are connected, the monitor gain is turned up and/or try a different lead
-
Continue CPR
-
Obtain IV access and administer adrenaline 1 mg immediately
-
Reassess the patient and rhythm every cycle (five sets of 30 compressions:2 breaths over approximately 2 minutes); remember to tell team prepare to defibrillate and use COACHED mnemonic:
- Defibrillate (delivering shock) or Dump charge
-
Give further adrenaline 1 mg IV every two cycles (approximately every 4 minutes)
-
Reassess the patient and rhythm every 2 minutes:
- If VF/pVT then switch to the shockable rhythm algorithm
- If pulse present, commence post-resuscitation care
-
Can consider:
- Atropine or cardiac pacing (non-invasive or invasive) in symptomatic severe bradycardia (percussion (fist) pacing may also be considered)
In All Cardiac Arrest/During CPR:
- Insert a LMA or ETT when practical and confirm placement with capnography
- Ventilate 10 times per minute once a definitive airway is in place without pausing for compressions and monitor using waveform capnography
- Verify ET position
- LMA insertion
- When an LMA can be inserted without delay it is preferable to avoid bag-mask ventilation altogether
- A size 5 will be correct for most men and a size 4 for most women
- Lubricate the outer face of the cuff area with a water-soluble gel
- Flex the patient’s neck slightly and extend the head
- Hold the LMA like a pen, insert it into the mouth and advance te tip behind the incisors with the upper surface applied to the palate until it reaches the posterior pharyngeal wall
- If possible, get an assistant to apply a jaw thrust after the LMA has been inserted into the mouth
- A slight 45 degree twist will often aid placement if intiial attempts at insertion beyond the pharynx are proving difficult
- Connect the inflating syringe and inflate the cuff with air (up to 40 mL for a size 5 LMA or up to 30 mL for a size 4 LMA) ⇒ the tube should lift 1-2cm out of the mouth as the cuff finds its correct position
- Confirm a clear airway by listening over the chest during inflation and observing bilateral chest movement
- With an LMA: attempt continuous uninterrupted compressions initally but abandon if persistent leaks and hypoventilation occur
- i-gel airway
- Size 4 will function well in most adults although small females may require a size 3 and a tall men a size 4
- Lubricate the back, sides and front of the i-gel cuff with a thin layer of lubricant
- Grasp the lubricated i-gel firmly along the integrated bite block and position the device so that the i-gel cuff outlet is facing towards the chin of the patient
- Ensure the patient is in the sniffing position (head extended and neck flexed) and gently press the chin down before inserting the i-gel
- If there is early resistance during insertion of the, get an assistant to apply a jaw thrust or rotate the device
- Give at least 20 mL of normal saline to flush any drugs administered and elevate the limb for 10-20 seconds to facilitate drug delivery to the central circulation but more practical to use a continuously running IV line than intermittent bolus flushing
- Establish a second IV line or establish Intraosseous Access
- Search and correct 4 Hs and 4Ts
- Consider bedside cardiac ultrasound during resuscitation to find potentially reversible causes
- Hypoxaemia: Deliver high-flow 100% oxygen and ensure ventilations create a visible rise and fall of both sides of the chest
- Hypovolaemia: Severe blood loss following surgery or internal haemorrhage and volume loss in anaphylaxis or sepsis may cause cardiac arrest
- Give fluid/blood replacement rapidly if hypovolaemia is likely and alert the relevant surgeon and theatre
- In the initial stages of resuscitation there are no clear advantages to using colloid: Use saline or Hartmann’s solution; Hartmann’s solution is preferred in trauma cases
- Ensure that the fluids are actually running
- Hyper/hypokalaemia, hypocalcaemia, acidaemia and other metabolic disorders
- Hyperkalaemia (>6.5)
- Give 10-20 mL of 10% calcium chloride solution IV immediately for hyperkalaemia (e.g. in renal patient who has a cardiac arrest)
- Do not give calcium solutions and sodium bicarbonate simultaneously by the same route, establish a second IV line
- Also give shifting agents (glucose 25 g + 10 units of short acting insulin)
- Calcium gluconate may be used in place of calcium chloride when its not available but calcium chloride is preferred because of its higher concentration of elemental calcium
- Consider 50 mL of 8.4% if the patient is severely acidaemic (pH<6.8) and is undergoing prolonged resuscitation or post-resuscitation care; or if there is hyperkalaemia
- Give 10-20 mL of 10% calcium chloride solution IV immediately for hyperkalaemia (e.g. in renal patient who has a cardiac arrest)
- Hypocalcaemia or calcium channel blocker overdose
- IV calcium chloride as above
- May occur in setting of shock, sepsis, pancreatitis and drug toxicities
- Hypokalaemia (<3.5)
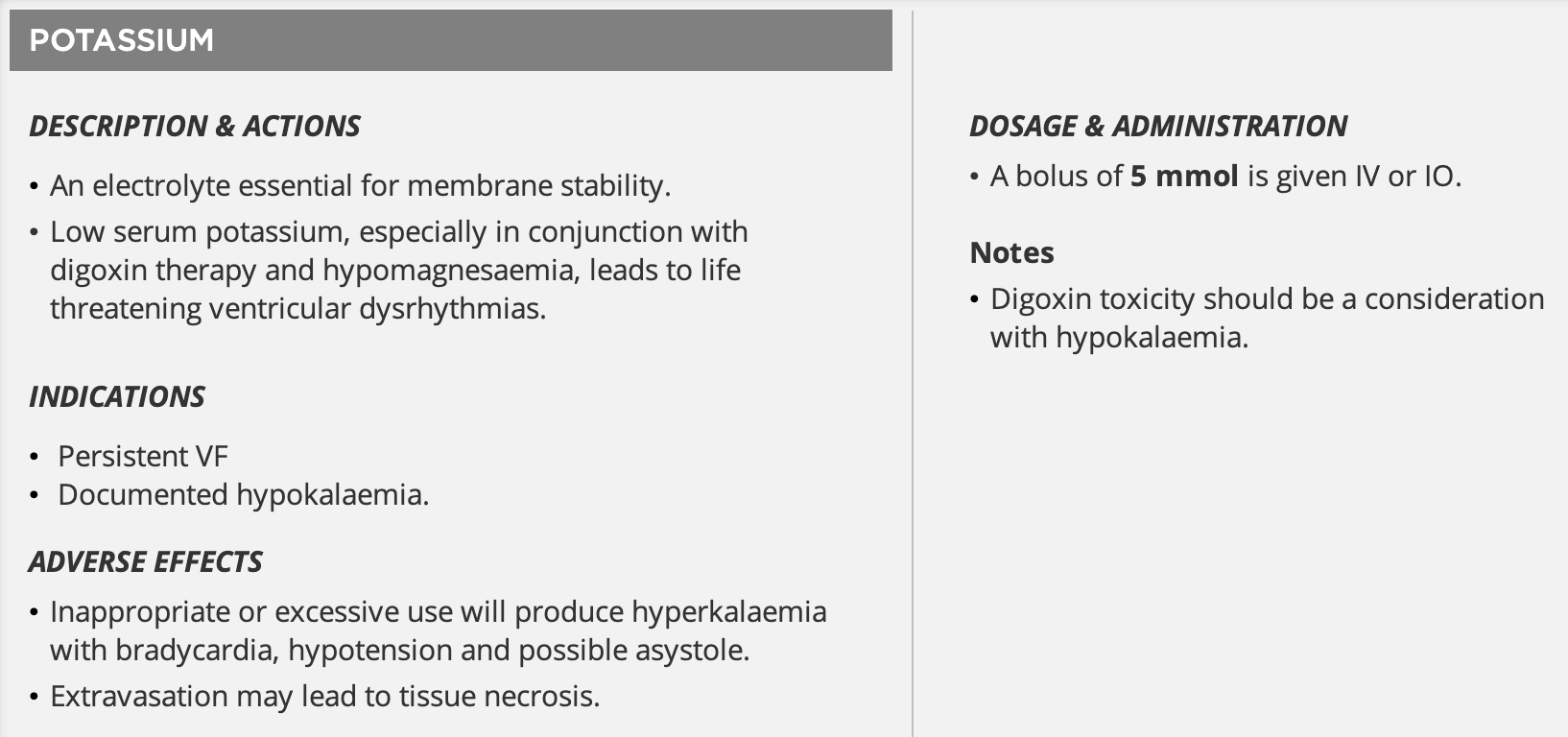
- Potassium 5 mmol IV as a bolus with a consideration for administration of magnesium sulflate 2g IV
- Hyperkalaemia (>6.5)
- Hypothermia
- Check core temperature
- Warm blankets, bair hugger, administration of warmed IV fluids, irrigation or gastric lavage with warmed fluids, bladder irrigation with warmed fluids
- Defibrillation cannot be performed on a patient with a core temperature ≤30°C; only CPR can be performed
- In patients <30°C; adrenaline administration time doubles (every 8 minutes) as reduced liver metabolism can cause adrenaline to accumulate
- Hyperthermia
- Active cooling techniques including cooling mats, wrapped ice packs, intravascular cooling techniques and IV fluids
- Malignant hyperthermia → dantrolene
- Tension pneumothorax
- Usually traumatic, particularly when the patient has positive-pressure ventilation
- Consider in cases such as: thoracic trauma, thoracic surgery or procedures (e.g. temporary pacing wire, existing chest drain, pacemaker/internal defibrillator implant, transthoracic needle aspiration or biopsy, subclavian or jugular vein catheterisation, thoracentesis, closed pleural biopsy), asthma, chronic obstructive pulmonary disease, pulmonary barotrauma
- Immediately insert a needle into the chest to decompress if there are asymmetrical chest movements and ventilation requires high pressures
- Immediate preparation for insertion of an intercostal drain/catheter is required
- Bedside ultrasound (eFAST)
- Clinical signs:
- Difficulty to ventilate
- Abnormal chest rise/fall on the affected side
- Decreased breath sounds on affected side
- Hyper-expanded chest with increased percussion note
- Tracheal deviation away from affected side
- Decompress rapidly by thoracostomy or needle thoracocentesis (using a 14g or larger long cannula/needle) into the second intercostal space at the midlcavicular line
- Tamponade
- Usually traumatic but may follow cardiothoracic surgery, MI etc.
- Signs include:
- Presence of elevated central venous pressure with neck vein distention
- Muffled heart signs
- Hypotension
- Intra-arrest ultrasound may be used to confirm diagnosis; freeze the image to avoid interrupting CPR as much as possible
- Perform pericardiocentesis if the patient is in cardiac arrest or peri-arrest
- Traumatic usually requires an emergency thoracotomy
- Toxins/poisons/drugs
- Specific antidotes such as naloxone, flumazenil, digoxin specific antibody fragments, phentolamine and glucagon are not proven to improve mortality when administered during cardiac arrest (except for cyanide poisoning)
- Adult patients with suspected severe cyanide poisoning should receive immediate parenteral hydoxocobalamin 5mg with repeat dosing up to 15mg
- In opiate induced respiratory arrest the dose of naloxone varies between small aliquots of 100 micrograms and a large 2mg dose aimed at achieving immediate and complete reversal
- Tricyclic toxicity, sodium bicarbonate bolus is the mainstay of therapy
- Specific antidotes such as naloxone, flumazenil, digoxin specific antibody fragments, phentolamine and glucagon are not proven to improve mortality when administered during cardiac arrest (except for cyanide poisoning)
- Thrombosis (PE or ACS)
- Perform vigorous external chest compressions to attempt to break up a massive PE when this is likely, and give a fluid load bolus of 20 mL/kg
- If high clinical suspicion of a massive PE (or ACS) causing cardiac arrest, a fibrinolytic agent can be given
- If a fibrinolytic drug is given in these circumstances consider performing CPR for at least 30 minutes and up to 60-90 minutes before termination of resuscitation attempts
- Monitoring during CPR
- Clinical signs such as breathing efforts, movements and eye opening can occur during CPR
- These can indicate ROSC and require verification by a rhythm and pulse check but can also occur because high quality CPR can generate sufficient circulation to restore signs of life including consciousness
- Carotid pulsation during CPR does not necessarily indicate adequate myocardial or cerebral perfusion in low cardiac output states
- Waveform capnography
- Normal end tidal is normally ~38 mmHg (35-45 mmHg)
- If ROSC is suspected during CPR by a significant increase in the end-tidal , then withold adrenaline; give adrenaline if cardiac arrest is confirmed at the next rhythm check
- Failure to achieve an end-tidal >10 mmHg after 20 minutes of CPR is associated with a poor outcome
- Clinical signs such as breathing efforts, movements and eye opening can occur during CPR
- Ultrasound during ALS
- A sub-xiphoid probe position is recommended
- Placement of the probe just before chest compressions are paused for a planned rhythm assessment is common place
- Stopping resuscitation:
- It is generally accepted that asystole for more than 20 min in the absence of a reversible cause and with ongoing ALS constitutes reasonable grounds for stopping further resuscitation attempts
- Consider following drugs (see Drugs in Cardiac Arrest):
Drugs to Consider During Arrest
- Drugs injected peripherally must be followed by a flush of at least 20 mL of fluid to facilitate drug delivery to the central circulation ⇒ more practical to use a continuously running IV line than intermittent bolus flushing
- In ventricular fibrillation/ventricular tachycardia (see below or see Drugs in Cardiac Arrest)
- Calcium: give 10 mL of 10% calcium chloride or 20 mL of 10% calcium gluconate IV for hyperkalaemia, hypocalcaemia or calcium-channel blocker overdose and repeat as necessary
- Lignocaine: initial bolus of 1 mg/kg IV for VF or pVT, when amiodarone is not available, followed by 0.5 mg/kg if necessary. Omit if amiodarone has been given
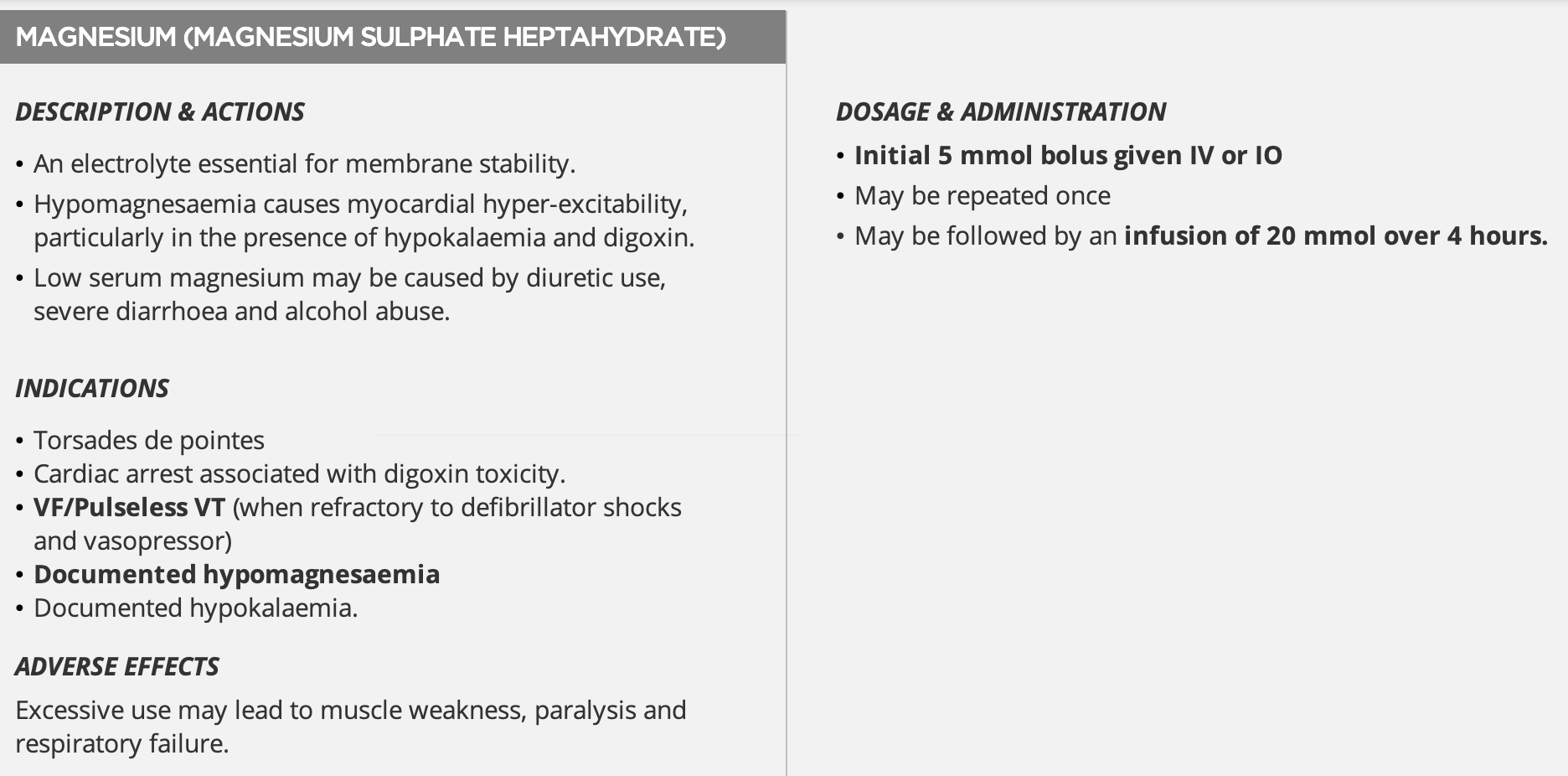
- Magnesium: give 2.5 g (10 mmol or 5 mL) of 49.3% magnesium sulfate IV in suspected hypomagnesaemia such as in patients with torsades de pointes, on potassium-losing diuretics or with digoxin toxicity
- Can repeat this bolus once and follow by an infusion of 20mmol over 4 hours (5mmol/h)
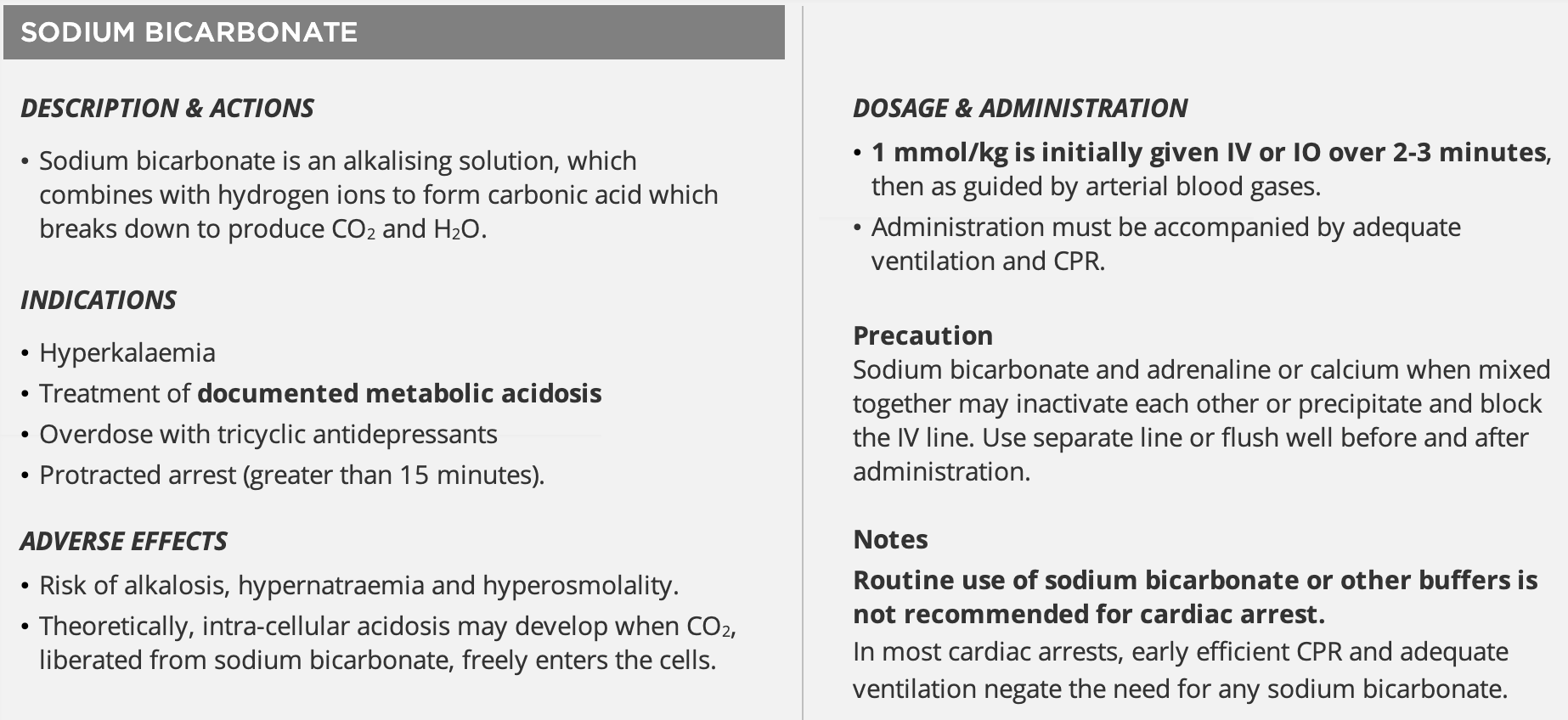
- Sodium bicarbonate: give 50 mmol of 8.4% (50 mL) IV boluses for hyperkalaemia, tricyclic antidepressant or other sodium-channel blocker overdose or severe metabolic acidosis or protracted arrest greater than 15 min
- Potassium: Give bolus of 5mmol IV for a low serum potassium especially when patient is on digoxin therapy or hypomagnesaemia
- In asystole or PEA
-
Make sure the ECG leads are not disconnected or broken by observing for compression artefact on the ECG screen during CPR

-
Check appropriate ECG lead selection and sensitivity
-
Consider atropine 1.0mg repeated to a maximum of 3mg for resistant asystole
-
Drugs in Cardiac Arrest
- See: ALS notes
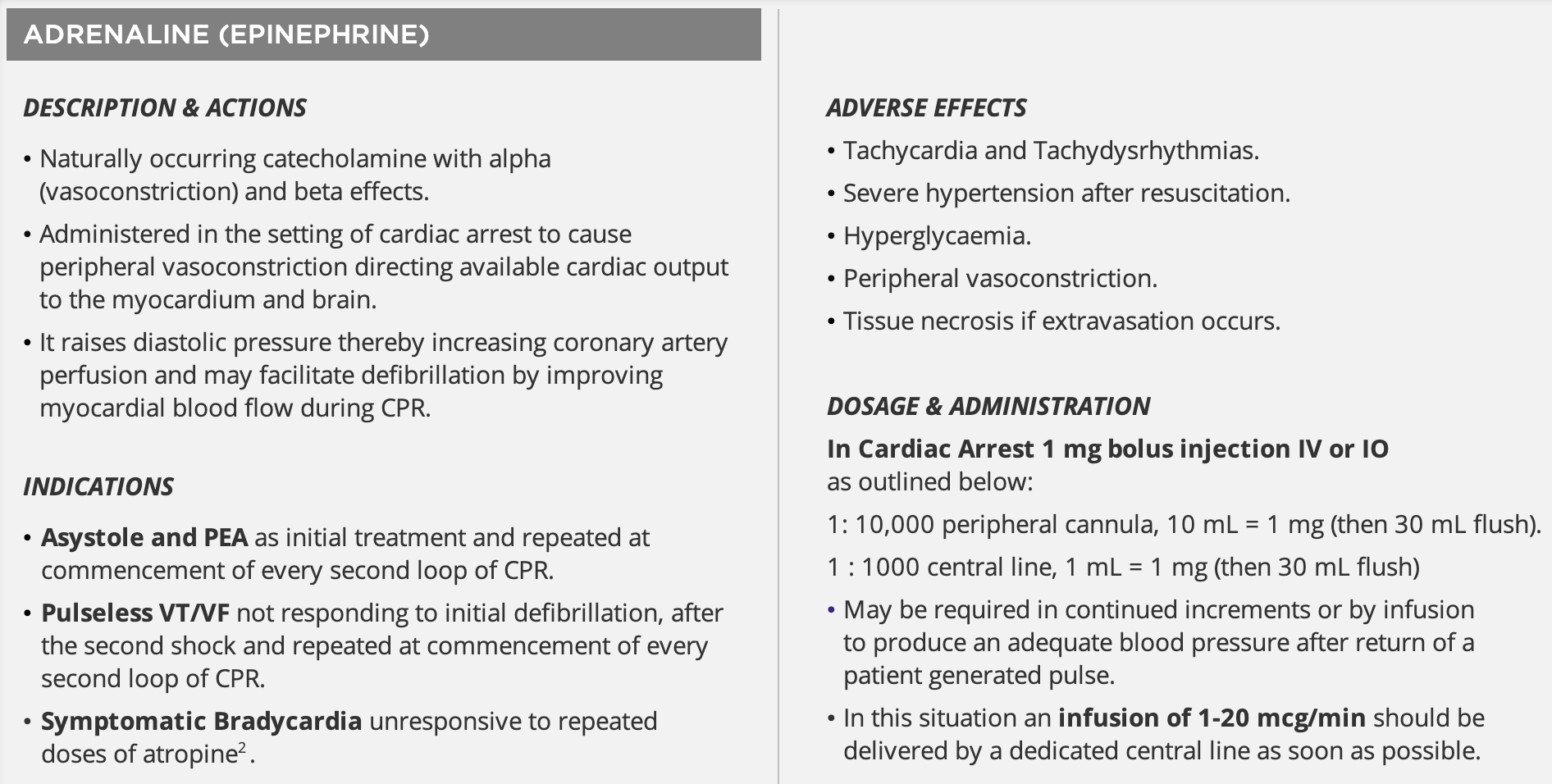
Adrenaline
- Indication: Cardiac arrest—give immediately if bradyasystolic rhythm or after the second shock if VF/pVT
- Cautions: Ensure reliable IV access; do not use cardiac arrest dose in a patient with a pulse.
- Comments: Can be given via intraosseous route if IV access not available.
- Dose: Available in 1 mg ampoules or rapid-access syringes (1:1000 (equivalent 1 mg/mL) and 1:10,000 ampoules (equivalent 0.1 mg/mL) concentrations)
- Adult:
- IV, intraosseous: 1 mg rapid IV (using 1 mL of 1:1000 solution or 10 mL of 1:10,000 solution) This is repeated every 3–5 min followed by a 20 mL normal saline flush to ensure central delivery of the drug (if using a peripheral vein)
- IV infusion: 1-4mcg/min; seek specialist advice
- Child:
- IV, intraosseous: 10mcg/kg (max: 1mg as single dose) repeat every 3-5 min
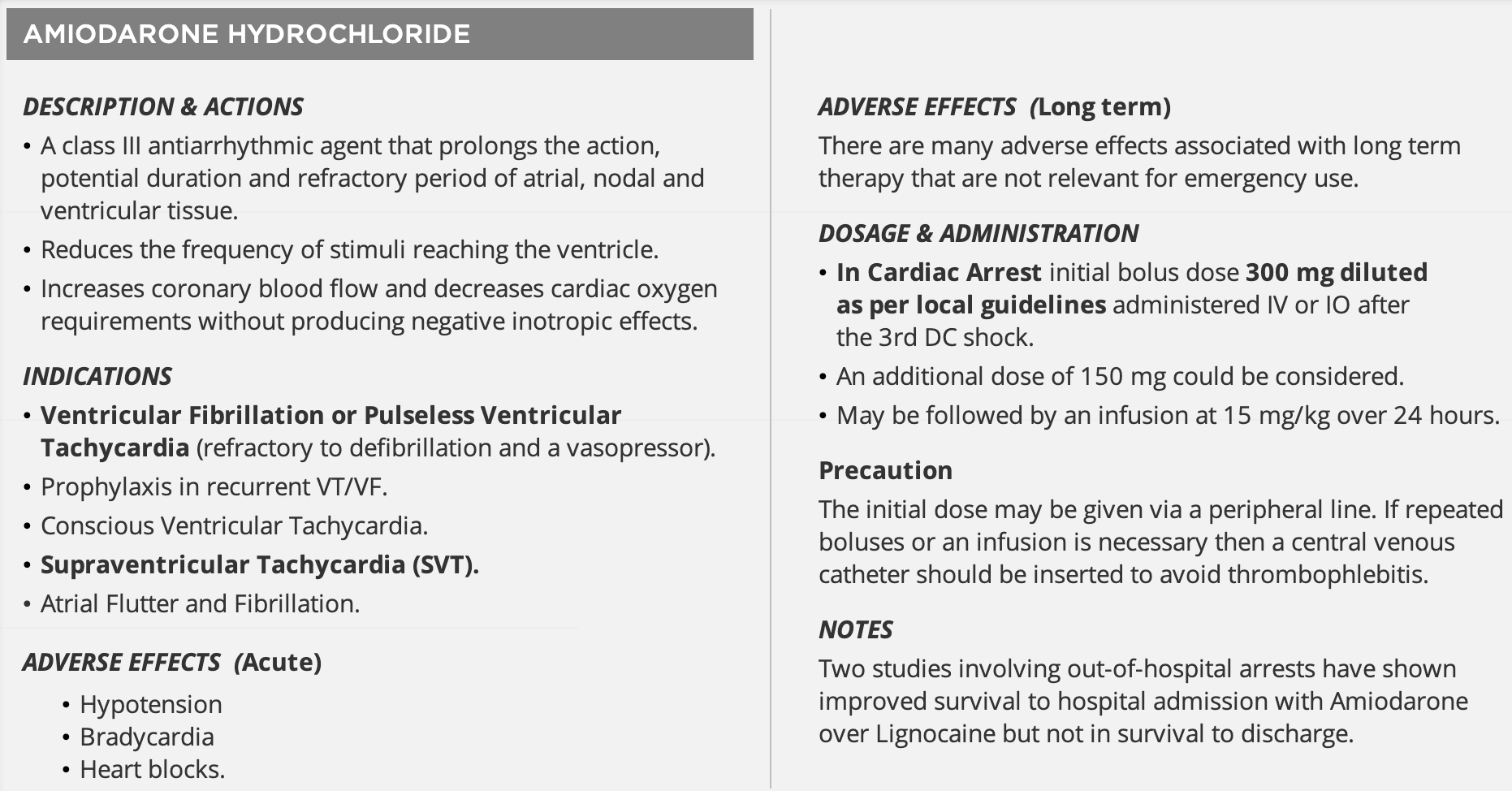
Amiodarone
- Also see: Antiarrhythmics
- Indication: Cardiac arrest—give following 3rd shock in refractory VF/pVT
- Adverse effects: may worsen bradyarrhythmias
- Cautions: Thrombophlebitis when injected into a peripheral vein. Not compatible with normal saline give with glucose 5%
- Comments: Can be given via intraosseous route if IV access not available - It is oily; shaking will cause bubbles and make it hard to draw up
- Dose: Available in 150 mg ampoules.
- Give amiodarone 300 mg (6mL) IV or IO diluted in 5% dextrose up to 20 mL over 1-2 mins after the third shock
- Flush with 5% dextrose or 0.9% sodium chloride, minimum of 20mLs
- Repeat 150 mg dose in 3–5 min if VF/pVT persists
- An infusion may be ordered after bolus dose(s) e.g. 15mg/kg over 24 hours
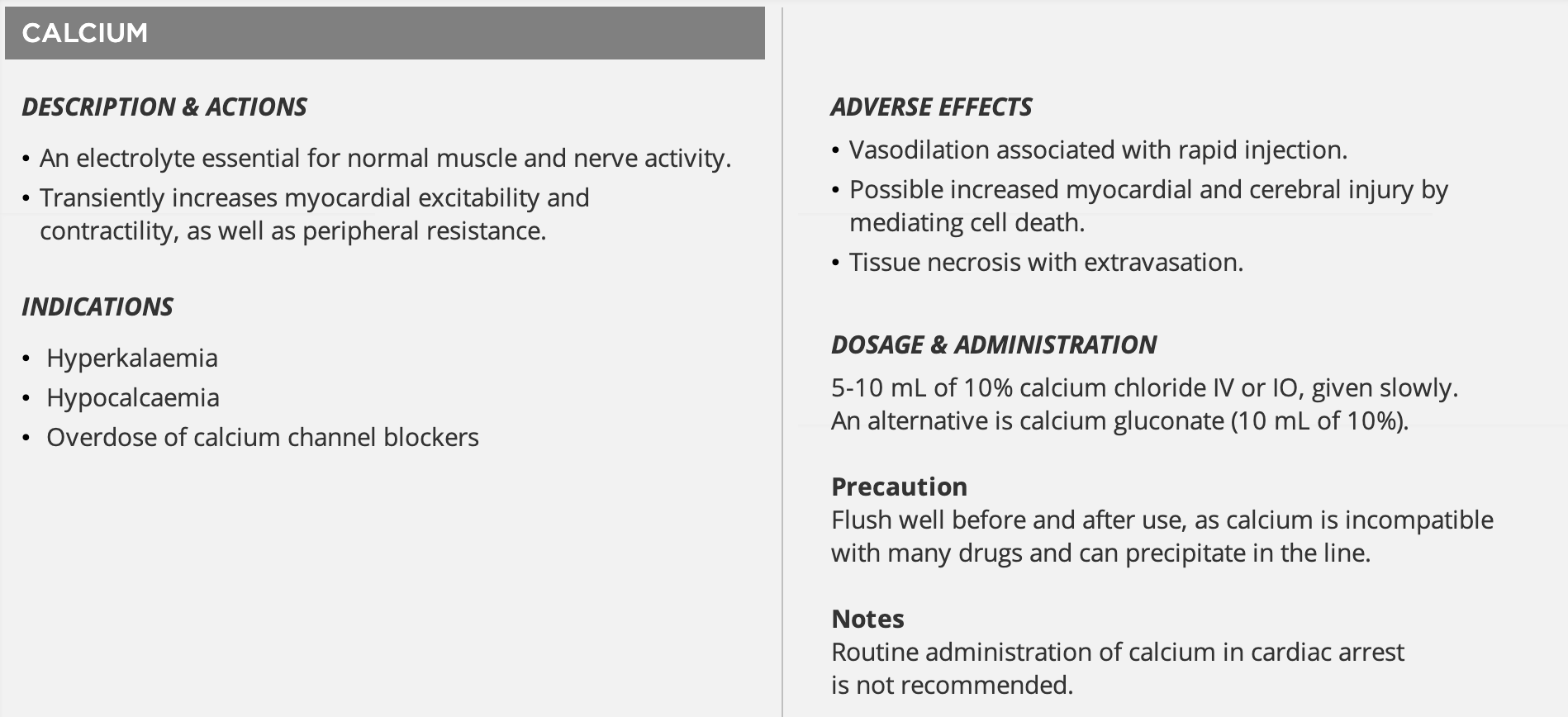
Calcium
- Indication: Cardiac arrest associated with hyperkalaemia (not due to digoxin toxicity), hypocalcaemia, calcium-channel blocker toxicity
- Cautions: Thrombophlebitis when injected into a peripheral vein. Not compatible with sodium bicarbonate → Do not give calcium solutions and sodium bicarbonate simultaneously by the same route
- Comments: Can be given via intraosseous route if IV access not available; flush well after use
- Dose: Available as 10% calcium chloride (6.8 mmol in 10 mL) and 10% calcium gluconate (2.2 mmol in 10 mL) ampoules
- Cardiac arrest: 10 mL of Ca chloride or 30 mL of Ca gluconate as rapid IV bolus. Repeat in 3–5 min if no response
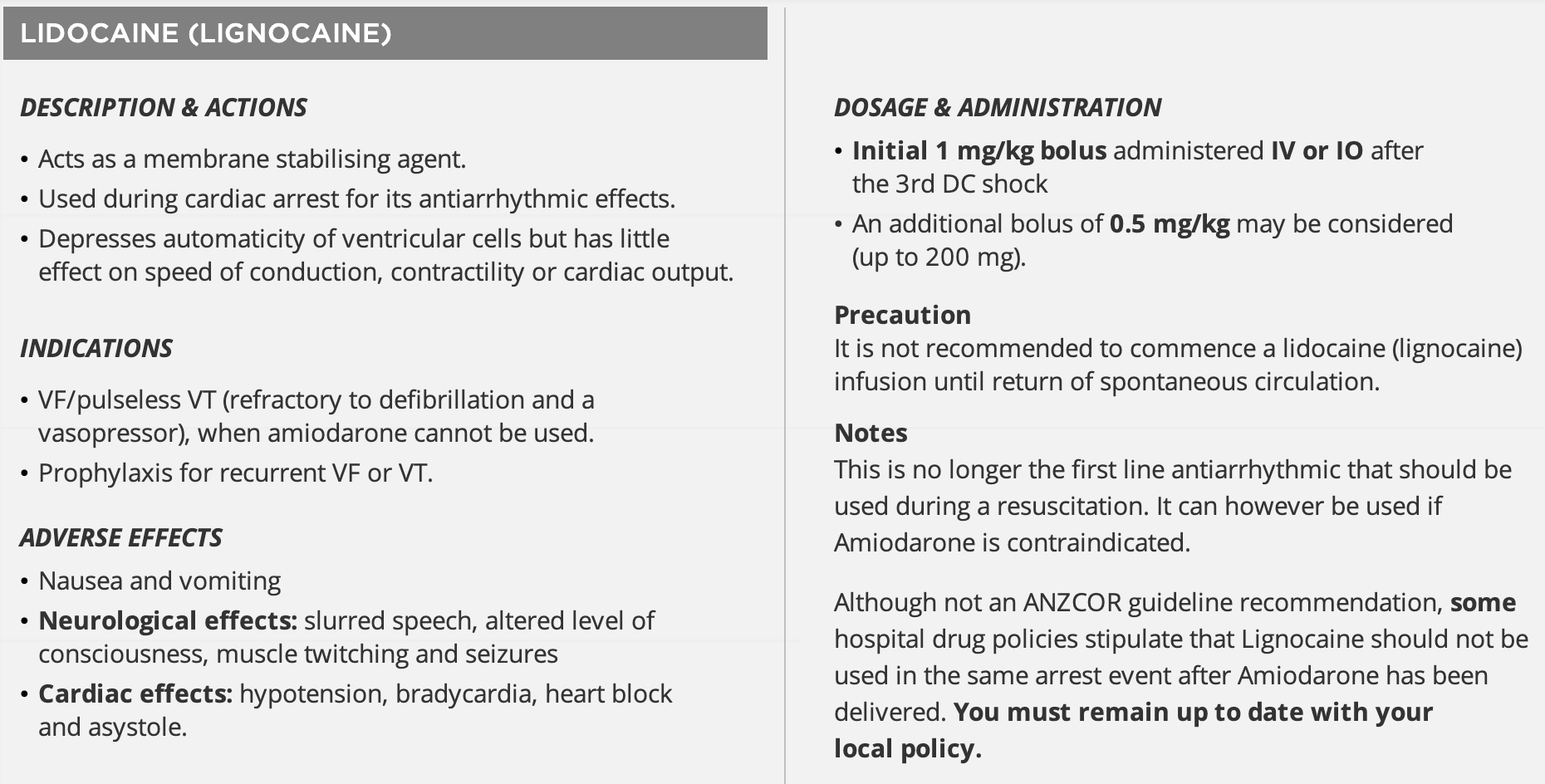
Lignocaine
- Indication: Cardiac arrest → give following 3rd shock in refractory VF/pVT if amiodarone unavailable
- Actions: Membrane-stabilising antiarrhythmic
- Adverse effects: Proarrhythmic → may worsen bradyarrhythmias
- Comments: Can be given via intraosseous route if IV access not available
- Dose: Available 100mg ampoules or rapid access syringes
- Cardiac arrest: 100mg rapid IV bolus. Repeat in 3-5 min if no response
Magnesium
- Indication: Cardiac arrest associated with hypomagnesaemia, torsades de points or digoxin toxicity; third line agent in refractory VF/pVT
- Comments: Can be given intraosseous route if IV access not available
- Dose: Available as 0% magnesium sulfate ampoules (2.g/10mmol in 5mL)
- Cardiac arrest: 10mmol rapid IV bolus. Repeat in 3-5 minutes if no response
Sodium Bicarbonate
- Indication: Cardiac arrest associated with hyperkalaemia, sodium channel blocker activity toxicity (TCA overdose) or severe metabolic acidosis, protracted arrest (>15 minutes)
- Cautions: Not compatible with calcium or adrenaline → Do not give simultaneously by the same route
- Comments: Can be given via intraosseous route if IV access not available
- Dose: Available in 100mL of 8.4% (100mmol) ampoules or 50mL of 8.4% (50mmol) rapid-access syringes
- Cardiac arrest: 50mmol rapid IV bolus. Repeat in 3-5 min if no response
Potassium
- Indication: Persistent VF, documented hypokalaemia
- Dose: Bolus of 5mmol is given IV or IO
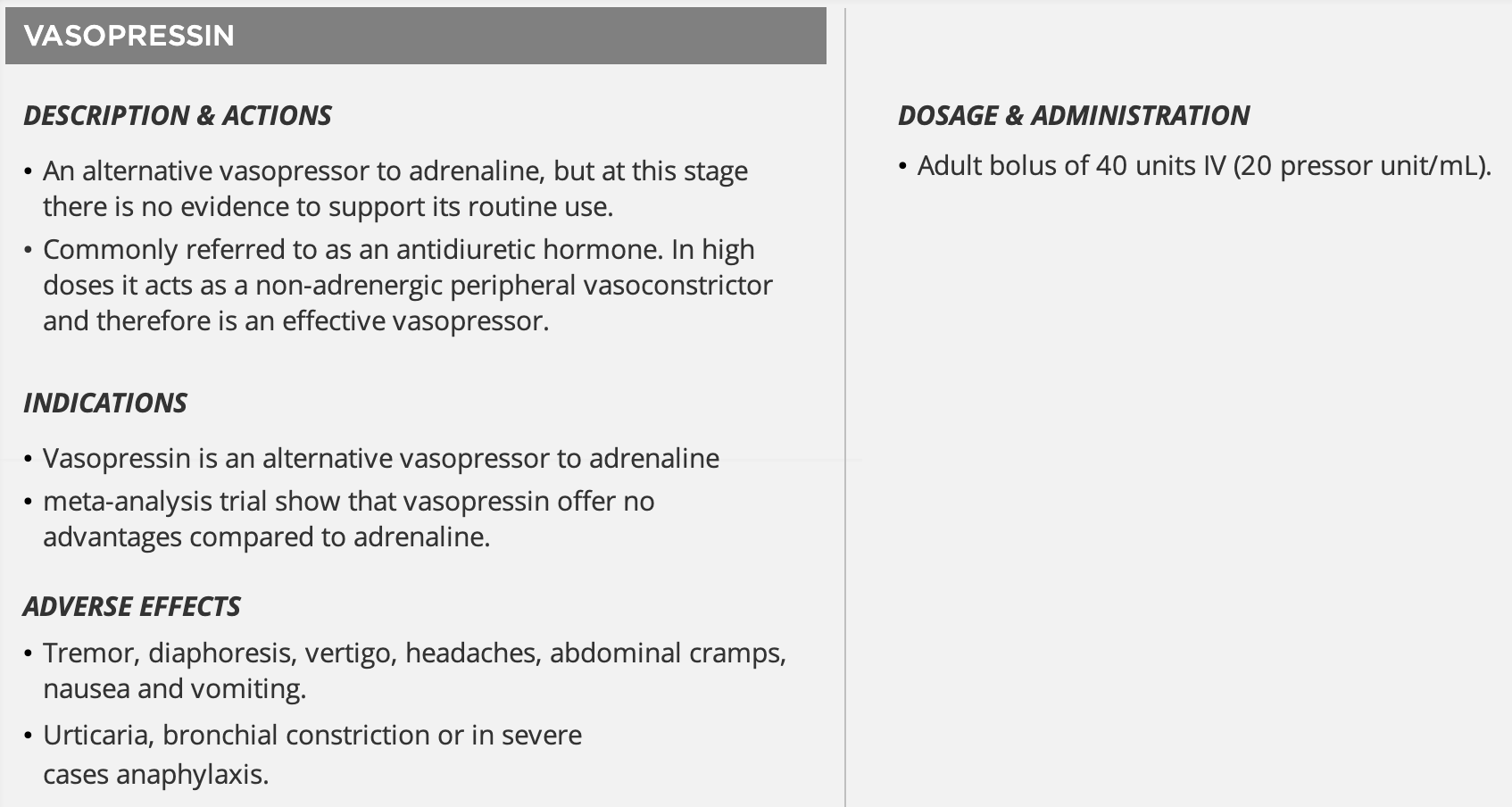
Vasopressin
Link to original
Closed Loop Communication
| Action | Individual | Example |
|---|---|---|
| Call out | Team leader | ”Steve, draw up adrenaline 1mg in 10mL of sodium chloride please” |
| Check back | Recipient (Steve) | “You want me to draw up adrenaline 1mg in 10mL of sodium chloride” |
| Closed loop | Team leader | ”Correct” |
Post Resuscitation Care
- Continue respiratory support
- Give supplemental oxygen, even if the patient has rapidly returned to consciousness
- Monitor ABG and titrate inspired oxygen to achieve oxygen saturations of 94-98%; hyperoxaemia after ROSC may be harmful
- Ventilation to maintain normocabia (Pa 35-45mmHg) should be achieved using ABGs as a guide rather than ET
- Ensure ETT is correctly positioned and secure and organise an immediate CXR
- Place NG tube to decompress the stomach if the patient is still comatose and/or intubated, confirming again with the CXR
- A→E assessment (including GCS)
- Maintain cerebral perfusion
- Maintain SBP >100 mmHg
- May require intermittent boluses of adrenaline 50-100 microgramss iV or an adrenaline infusion under close supervision
- Ensure there is adequate intravascular volume by looking for sources of hypovolaemia, checking JVP or arranging for the insertion of a CVL
- Treat and prevent cardiac arrhythmias
- Treat and prevent cardiac arrhythmias
- Infusions of amiodarone may be used as prophylactic therapy for suspected recurrent VT
- Repeat investigations: including a 12-lead ECG, blood glucose, ABG or VBG and electrolytes
- Avoid hypo-/hyperglycaemia or acidosis and control seizures
- Hyperglycaemia is associated with poor neurological outcome; treat BGL >10mmol/L with insulin
- Commence targeted temperature management
- Cool patients to between 32°C to 34°C for a period of 12-24 hours
- Initially induced by the rapid infusion of ice cold fluids or icepacs to reduce the core temperature
- If not using targeted temperature management, fever should be avoided and a target temperature of 36°C should be aimed for
- Cool patients to between 32°C to 34°C for a period of 12-24 hours
- Seek and treat underlying cause of the cardiac arrest or any complications of the resuscitations (e.g. pneumothorax from a broken rib or pulmonary aspiration)
- Consider seizure prophylaxis
- Consider immediate coronary angiography and PCI especially for patients following chest pain or with ST elevation
- Transfer to ICU, cardiac catheter lab or CCU
Footnotes
-
Asystole only when fine VF cannot confidently be excluded. Immediate high quality CPR may increase the amplitude and frequency of the VF making the diagnosis clear and increasing the probability of successful defibrillation ↩
-
VF may be confused for supraventricular tachycardia with aberrancy. In the case where it leads to clinical cardiac arrest, the correct treatment is immediate defibrillation so misinterpretation as VF (or even VT) would not lead to inappropriate treatment ↩
-
This is because even if the defibrillation attempt is successful in restoring a perfusing rhythm, it is very rare for a pulse to be palpable immediately after defibrillation. The time until ROSC can be longer than two minutes in as many as 25% of successful shocks. The delay in trying to palpate a pulse will further compromise the myocardium if a perfusing rhythm has not been restored. Even if a perfusing rhythm has been restored has been restored, giving chest compressions does not increase the chance of VF recurring ↩
-
Pulseless narrow complex tachycardia is considered PEA, but immediate management is CPR and synchronised cardioversion at 200J as soon as possible ↩