Presentation
- Pain is sharp, retrosternal and radiates to the back; worse on inspiration, swallowing or lying down and relieved by sitting up
- Pericardial rub best heard along the left sternal edge in expiration with the patient sitting up; but may be transient
- Pericarditis 2° TB, uraemia or neoplastic disease is more insidious and ±pain; patients present with insidious pericardial tamponade
Diagnosis
- Diagnosed when ≥2 of the following:
- Pericarditic chest pain
- Pericardial rubs on auscultation
- New widespread ST elevation or PR depression on ECG
- Pericardial effusion (new or worsening)
Management
- Attach cardiac monitoring and pulse oximeter to the patient
- Send bloods for FBC, UEC, LFTs, troponin and viral serology
- CRP, ESR and WCC may be raised as markers of inflammation
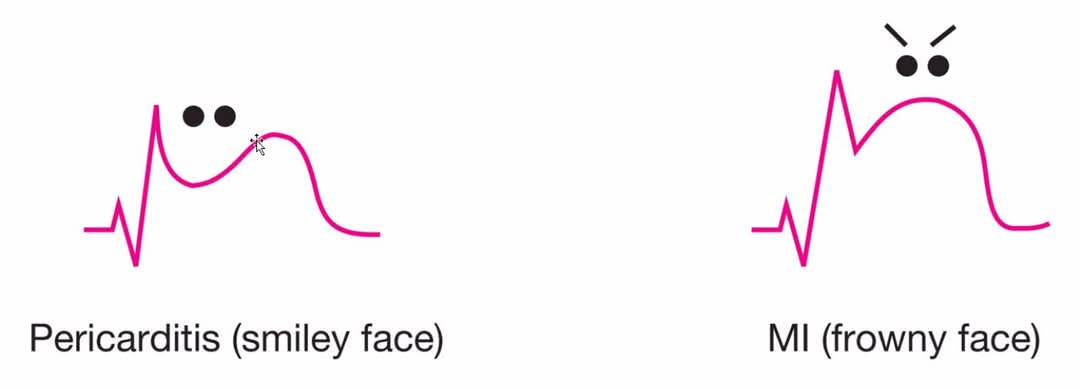
- ECG may show:
- Sinus tachycardia alone
- Widespread concave ST elevation or PR-segment depression
- Later T waves may flatten or become symmetrically inverted
- May show features of pericardial effusion:
- Decreased voltages
- Electrical alternans
- Request CXR
- Normal usually
- Transthoracic echocardiogram
- Arrange an urgent echocardiogram and pericardiocentesis if signs of cardiac tamponade:
- Tachycardia
- Hypotension
- Pulsus paradoxus
- Raised JVP that rises on inspiration
- Otherwise echocardiogram organised electively1
- Arrange an urgent echocardiogram and pericardiocentesis if signs of cardiac tamponade:
- Admit the patient if a treatable cause is found or if any of the following:
- High fever >38°C
- Large pericardial effusion
- Cardiac tamponade
- Failure to respond within 7 days to drug therapy
- Other considerations that might influence admission: myopericarditis, immunosuppression, trauma and oral anticoagulant therapy
- Specific management if appropriate (e.g. connective tissue disorder → immunosuppression, uraemia → dialysis)
- Non-pharm
- Restrict exercise
- Pharm
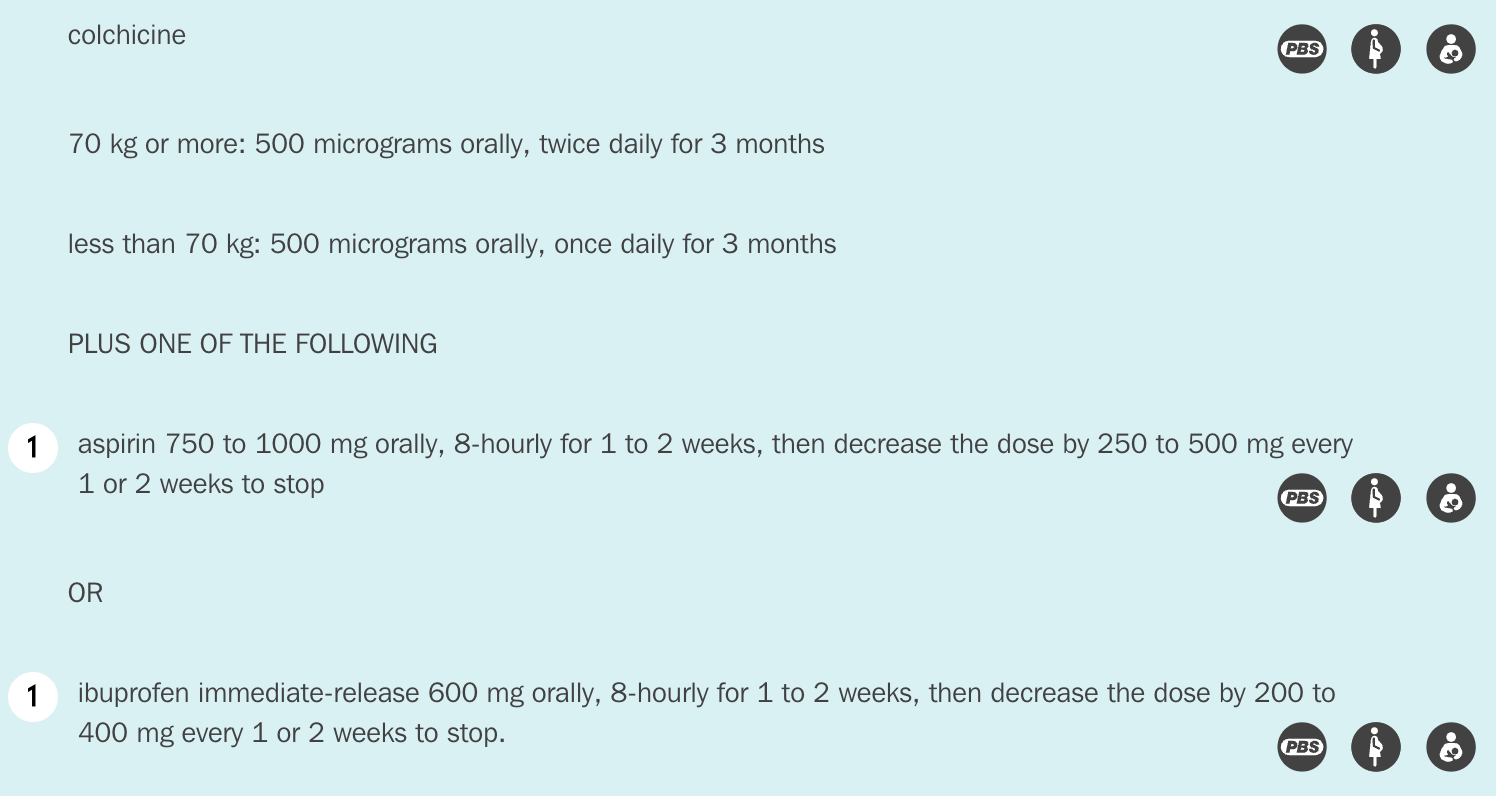
- Colchicine; does not need tapering to stop
- NSAID (usually aspirin) for 1-2 weeks as guided by symptom resolution and normalisation of inflammatory markers; consider tapering to stop
Warning
Must distinguish from STEMI because thrombolysis is contraindicated in pericarditis due to risk of bleeding from haemorrhagic transformation
Footnotes
Footnotes
-
eTG suggests to arrange a TTE for all patients with pericarditis, but on call only suggests to arrange for patients with suspected pericardial effusion ↩