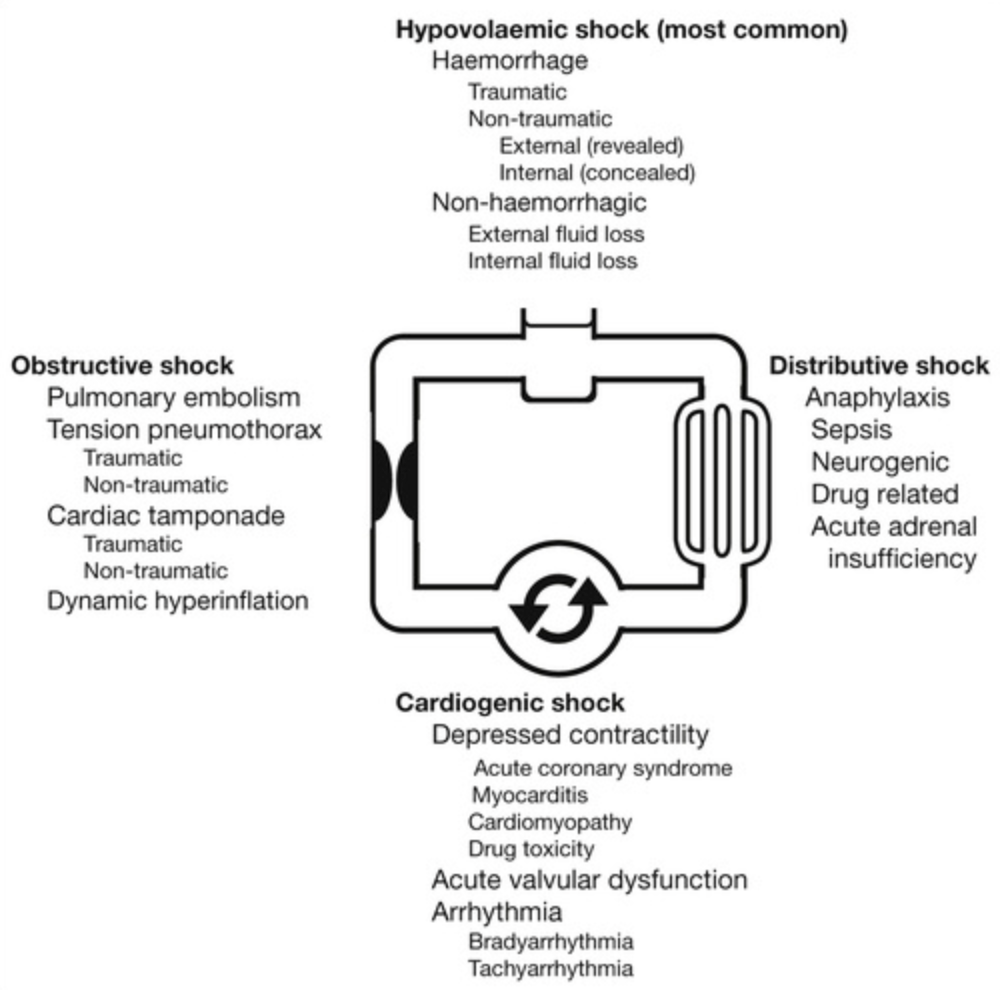
Causes
Classification
- Hypovolaemic shock
- Haemorrhagic
- Traumatic: external or internal (e.g. haemothorax, haemoperitoneum, retroperitoneal haemorrhage)
- Non-traumatic: external (e.g. haemoptysis, haematemesis, PV bleeding) or internal (e.g. haemothorax, ruptured AAA, bleeding diathesis)
- Non-haemorrhagic
- External (e.g. GI losses from diarrhoea and vomiting, burns, hyperthermia, high-output fistulae)
- Internal (e.g. bowel obstruction, pancreatitis)
- Haemorrhagic
- Cardiogenic shock
- Depressed contractility: ACS, myocarditis, myocardial contusion, cardiomyopathy, drug overdose (e.g. CCB or beta-blocker)
- Acute valvular dysfunction: Papillary muscle or chordae tendinae rupture, infective endocarditis, severe aortic stenosis or mitral stenosis
- Arrhythmia: Tachycardia (e.g. VT, AF, SVT), bradycardia (e.g. heart block)
- Distributive shock
- Anaphylaxis
- Sepsis
- Neurogenic: Loss of sympathetic tone from high spinal cord trauma or epidural anaesthesia
- Drug related: Vasodilator antihypertensive agents, nitrates, strong analgesics
- Acute adrenal insufficiency: Addison’s disease, discontinuing long-term steroids
- Obstructive shock
Assessment
- Identify the possible cause as above, assessing volume status and JVP and examining the ECG
- A low/non-visible JVP suggests hypovolaemic or distributive shock
- A raised JVP is seen in cardiogenic and obstructive shock
- ECG changes may be the cause or the effect of the shock state
- Look at the colour of the hands and digits and feel the temperature of the patient’s hands
- Skin and mucous membranes
- An adequately hydrated patient has moist mucous membranes and a small pool of saliva at the undersurface of the tongue in the area of the frenulum
- Check tissue turgor by raising a fold of skin from the anterior chest area over the sternal angle
- Measure CRT, HR, SBP and pulse pressure (widens in distributive and narrows in hypovolaemic), JVP
- Check postural HR and BP and repeat the HR and BP after the patient sits or stands for at least 2 minutes
- An increase in HR >20 beats/min, a fall in SBP >20 mmHg or any fall in DBP indicates postural hypotension
- Assess the capillary refill time by pressing on a nailbed (held at the level of the heart) for 5 seconds. Over 2 seconds is regarded as prolonged
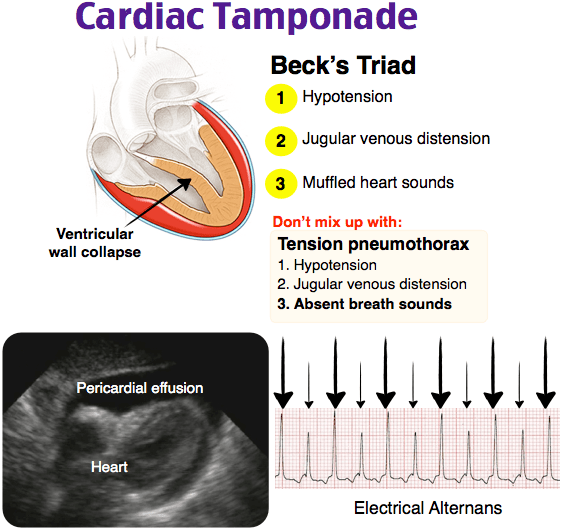
- JVP usually falls on inspiration but Kussmaul’s sign is when JVP rises on inspiration seen in cardiac tamponade
- Low diastolic blood pressure suggests arterial vasodilation as in Anaphylaxis or Sepsis
- A narrowed pulse pressure (<35-45 mmHg) suggests arterial vasoconstriction (cardiogenic shock or hypovolaemia)
- Check postural HR and BP and repeat the HR and BP after the patient sits or stands for at least 2 minutes
- Measure urine output
- Oliguria (urine volume <0.5 mL/kg/h)
- Volume overload features:
- Raised JVP, peripheral oedema (taut, non-compliant skin), enlarged tender liver with positive hepatojugular reflux (liver pressing causes persistent elevation in JVP)
- An S3 gallop, lung crackles or pleural effusion
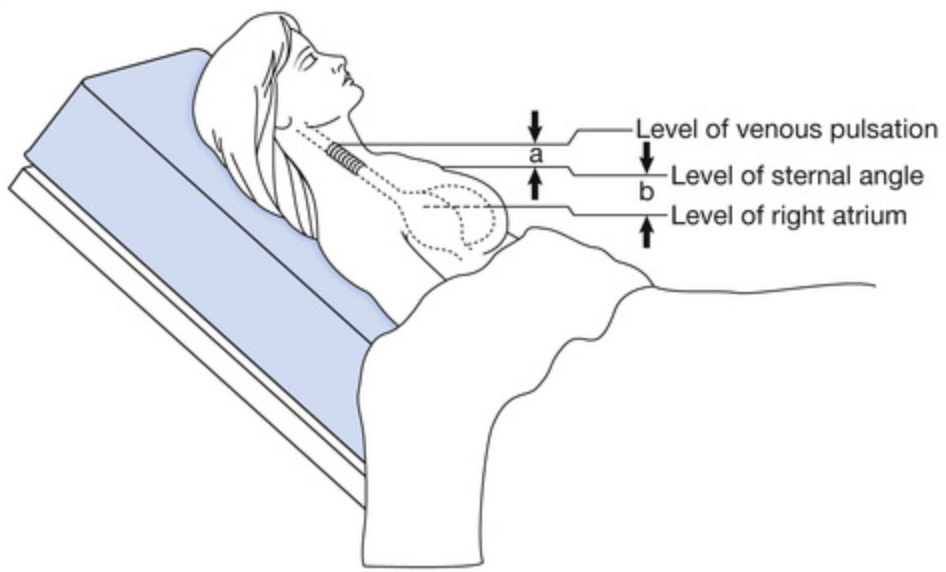
Measuring JVP
- Can actually be done at any angle from 0 to 90 degrees. We often start at 45 degrees but if you can’t see it, the JVP is either low in which case lower the head of the bed or the JVP is high in which case raise the head of the bed
- Once identified measure the perpendicular distance above the sternal angle to the top of the column of blood
- A JVP of 2-3 cm above the sternal angle is normal in adult patients; volume-overloaded patients have a JVP >3cm
- Pressing on the abdomen induces the hepatojugular reflux which increases the level of the JVP which may make it easier to identify
Management
- Give oxygen and rapid IV fluid replacement (provided no evidence of cardiac failure)
- Maintain SpO2>95%
- Known COPD and modifications to obs. chart then can titrate the SpO2
- Call early for a senior doctor to help
- Start monitoring
- Pulse oximetry, ECG, BP, urine output, invasive arterial and venous monitoring if in ICU
- Optimise oxygenation and ventilation:
- Consider high-flow oxygen and assisted ventilation if necessary
- Optimise heart rate and rhythm:
- Cardioversion of a cardiac tachyarrhythmia if causing hypotension
- Atropine, adrenaline and pacing if bradycardia causing hypotension
- Optimise preload and haemoglobin:
- Give 10-20 mL/kg normal saline rapidly IV and repeat until JVP is 3-5 cm above the sternal angle
- Do not give fluids if JVP is already raised and the patient is in pulmonary oedema
- If more than 60 mL/kg is required, check Hb to determine need for blood transfusion
- Give blood early for ongoing haemorrhage and arrange urgent surgery according to the cause; aim for Hb >90-100 g/L
- Give 10-20 mL/kg normal saline rapidly IV and repeat until JVP is 3-5 cm above the sternal angle
- Optimise afterload:
- Give a vasopressor if vasodilated from Anaphylaxis or sepsis (e.g. adrenaline or noradrenaline respectively)
- Do not use a vasopressor in hypovolaemia (especially haemorrhagic shock)
- Optimise cardiac function:
- Inotropic support (e.g. low-dose adrenaline, dobutamine or dopamine infusion) if still shocked despite above measures
- Treat sepsis:
- Give broad-spectrum antibiotics early if septic shock is suspected
Fluid replacement in dehydrated patients
- Resuscitate intravascular volume until perfusion is normalised as above with 20 mL/kg boluses of crystalloid (normal saline preferred)
- Calculate fluid losses (generally at least 10% of body weight if patient is dehydrated and hypotensive, i.e. 70kg patient is depleted of 7L of fluid)
- Subtract from this defecit the amount of fluid already given for resuscitation (e.g. if 2L given during resuscitation, a 70kg patient still requires 5L of fluid)
- Replace this amount over the next 24 hours together with maintenance fluid and ongoing losses
- Use 4:2:1 rule, or add 60mL to their weight for hourly fluid requirement ⇒ 110mL/hr ≈ 2.5L/day
- Total fluid to be replaced is 7.5 L
- Replace half in first 8 hours and remainder in next 16 hours
- 3.75L over 8 hours ≈ 450 mL/h
- 3.75L over 16 hours ≈ 230 mL/h
- Monitor adequacy of replacement by perfusion and vital signs, urine output and electrolyte changes
- Crystalloids (e.g. normal saline) are widely used as fluid replacement
- Normal saline has a half-life in the intravascular space of around 1-3 hours
- Colloids stay in the intravascular space for longer
- Albumin has a half-life in the intravascular space of around 17-20 hours
- They are more expensive and may cause allergic reactions
- 5% dextrose equilibrates across the intravascular, interstitial and intracellular spaces and does not support the intravascular volume and therefore has no role in fluid resuscitation in shock