Phone Call/Presentation Questions
- SOCRATES of the pain
- Character of the pain
- How severe is the pain
- Where is the main site of pain; is it localised or generalised
- Changes in vital signs such as fever, tachycardia or hypotension?
- Associated symptoms (e.g. nausea, vomiting, distention, constipation or dysuria)
- Has the patient had past or recent abdominal surgery?
- What was the reason for admission?
- Is the patient on steroids or immunosuppressed?
- Is this a new problem? Has it occurred before?
Common Causes (Corridor Thoughts)
- Can be broadly grouped into surgical and medical
Medical Causes of Acute Abdominal Pain
- Thoracic
- MI, pericarditis
- PE, pleurisy, pneumonia
- Aortic dissection
- Abdominal
- Hepatitis, right heart failure
- Infection including gastroenteritis, pyelonephritis, cystitis, bacterial colitis and peritonitis
- Intestinal ischaemia from atheroma, vasculitis, Henoch–Schönlein purpura or sickle cell disease
- Reflux, peptic ulcer disease, inflammatory bowel disease
- Endocrine and metabolic
- DKA
- Addison’s disease
- Hypercalcaemia
- Lead poisoning, paracetamol or iron poisoning
- Neurogenic
- Herpes zoster
- Radiculitis from spinal cord pathology
- Tabes dorsalis
- Thoracolumbar spine
- Collapsed/fractured vertebra from osteoporosis, neoplasm or infection (e.g. TB)
Surgical Causes of Acute Abdominal Pain
- Gastrointestinal
- Oesophageal cancer
- Gastric cancer
- Gallbladder: biliary colic, acute cholecystitis, ascending cholangitis
- Pancreatitis
- Liver: subphrenic abscess, hepatic abscess
- Spleen: rupture, abscess
- Small intestine: intussusception, obstruction, perforation, ischaemia
- Large intestine: obstruction, perforation, diverticulitis, ischaemic colitis
- Appendix: appendicitis, appendacaecal abscess
- Mesenteric adenitis
- Hernia
- Urological
- Renal: renal colic, ureteric colic
- Bladder: urinary retention
- Testicles: torsion, epididymitis, cancer
- Vascular:
- AAA
- Gynaecological:
- Uterine: bleed into fibroid, pregnancy-related
- Ovarian: torsion, ruptured cyst, haemorrhage, cancer
- Fallopian tube: Ectopic pregnancy, pelvic inflammatory disease
- Mittelschmerz, endometriosis
- Musculoskeletal
- Rectus muscle haematoma or tear
Major Threat to Life
- Exansanguinating haemorrhage with hypovolaemic shock
- Leaking AAA, ruptured ectopic pregnancy or splenic rupture
- Consider iatrogenic causes (e.g. liver or renal biopsy, thoracocentesis)
- Perforated viscus
- Rigid abdomen with severe pain
- Necrosis of viscus
- Severe pancreatitis, intussusception, volvulus, strangulated hernia or ischaemic colitis can rapidly cause hypovolaemic or septic shock and electrolyte and acid-base disturbances
- Intraperitoneal septic focus
- Infection from a localised site such as ascending cholangitis or an infected obstructed kidney may progress to generalised septic shock within hours
- Extra-abdominal causes
- Patients with AMI, thoracic aortic dissection and/or DKA may present with acute abdominal pain
Assessment
End of Bed
- Patients with severe colic are often restless and writhing in discomfort
- Patients with peritonitis lie still avoiding any movement
A to E Assessment
- Heart rate and blood pressure?
- Tachycardia (HR >120) + Hypovolaemia (SBP <90mmHg) is associated with shock
- Sudden abdominal pain associated with hypotension consider: inferior MI (do ECG), pancreatitis (measure lipase), ruptured AAA or ectopic pregnanct (urgent USS/FAST) and mesenteric infarction (bloody diarrhoea with a metabolic acidosis and raised lactate)
- Gradual onset abdomen with hypotension consider: peritonitis, perforation or urosepsis
- Recheck the BP and HR with the patient standing if the supine BP is normal ⇒ A ↓ BP with ↑ HR (>20 beats/min) ⇒ underlying hypovolaemia
- Respiratory rate?
- Shallow, rapid breathing consider generalised abdominal pain, peritonitis or subdiaphragmatic irritation
- Sustained tachypnoea is associated with sepsis, metabolic acidosis, anaemia, pneumonia and CCF
- Temperature?
- Fever consider infection or inflammation
Selective History and Chart Review
- Ruptured AAA
- Patients are usually elderly and complain of sudden, severe low abdominal, back, flank or groin pain, sometimes associated with syncope
- The pain may mimic ureteric colic
- Onset gradual or sudden?
- Sudden onset ⇒ Perforation of a viscus, ruptured ectopic pregnancy, torsion of an ovarian cyst or a leaking AAA
- Severe pain in waves that develops over minutes to hours ⇒ colic (renal, biliary or intestinal)
- Character?
- Burning ⇒ peptic ulcer
- Sharp and constricting (‘takes one’s breath away’) ⇒ Biliary colic
- Deep and agonising, eased by sitting forwards ⇒ Acute pancreatitis
- Gripping with intermittent exacerbations ⇒ Bowel obstruction
- Relentness and worsened on coughing or moving; the patient prefers to lie still ⇒ Peritonitis
- Patient rolls around trying to get comfy ⇒ Ureteric colic
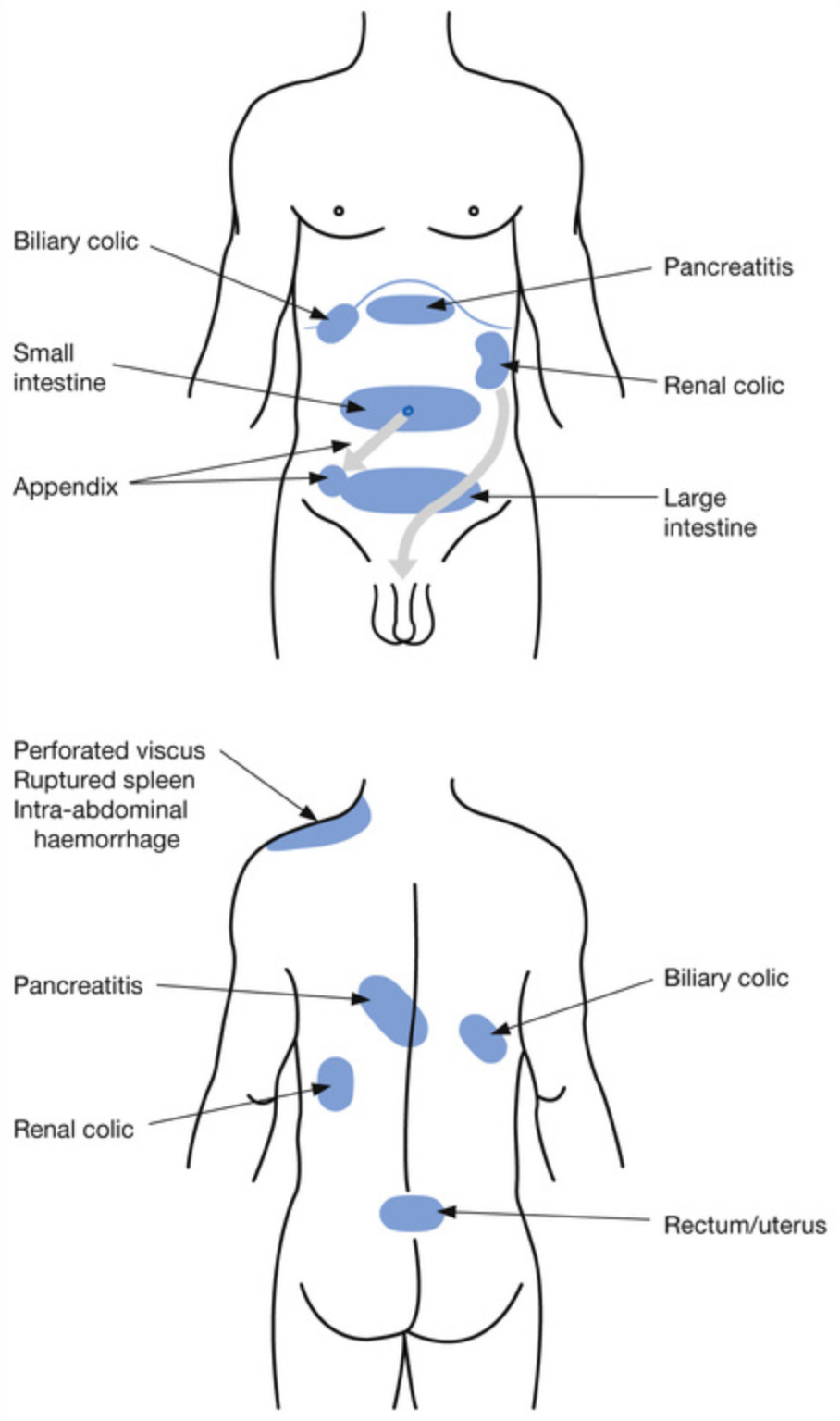
- Location?
- May need to find localisation by examination
- Does the pain radiate
- Has the pain changed since onset?
- A ruptured viscus is initially associated with localised pain that subsequently shifts or becomes generalised
- Aggravating or relieving factors?
- Duodenal ulcer pain is often relieved by the ingestion of food.
- Pancreatitis pain is worsened after eating and may be relieved by sitting up or leaning forwards
- Pain that increases with inspiration suggests biliary origin, peritonitis or pleurisy
- Pain associated with frequency and dysuria aggravated by micturition suggests a urological cause
- Pain worse with movement such as coughing is usually secondary to localised or generalised peritonitis (e.g. appendicitis)
- Pain relieved by movement or that makes the patient restless is more often colicky in nature (e.g. ureteric colic)
- Other associated symptoms?
- Nausea or vomiting?
- Pain prior to nausea and vomiting ⇒ surgical acute abdomen
- Pain following nausea and vomiting ⇒ gastritis or gastroenteritis
- Vomiting that occurs at the onset of pain ⇒ peritoneal irritation, perforation of a viscus, acute pancreatitis or a high intestinal obstruction
- Vomiting many hours after the onset of abdominal pain may be caused by lower intestinal obstruction or ileus
- Vomiting after fasting ⇒ gastric stasis or gastric outlet obstruction
- Contents of vomiting?
- Clear fluids ⇒ obstruction proximal to sphincter of Oddi in the second part of the duodenum
- Faeculent vomit ⇒ distal intestinal obstruction or a gastrocolic fistula
- Blood ⇒ see Haematemesis
- Frequency and character of stool?
- Bloody diarrhoea with abdominal pain ⇒ invasive enteritis (e.g. Shigella and Salmonella), ischaemic colitis and inflammatory bowel disease
- Diarrhoea alternating with constipation ⇒ diverticular disease, colonic neoplasm
- Absolute constipation with lack of flatus ⇒ low large bowel obstruction or ileus
- Fever or chills?
- Check temperature record since admission and check medication sheet for antipyretic or steroid use which may mask a fever
- Nausea or vomiting?
- Documentation review
- Is there a history of abdominal pain?
- Consider: Gastritis or oesophageal reflux, peptic ulcer disease, alcoholic pancreatitis, cholelithiasis, uretoerolithiasis
- Is there a history of previous abdominal surgery? ⇒ adhesions
- Recent history of blunt trauma to the abdomen
- Contained subcapsular haematoma of the spleen may rupture several days later
- Abnormal spleen in infectious mononucleosis, malaria or a lymphoproliferative disorder can rupture with minimal or even no obvious trauma
- Is there a history of chronic liver disease from alcohol, viral hepatitis or non-alcoholic steatohepatitis (NASH)
- Always consider spontaneous bacterial peritonitis in a patient with chronic liver disease, ascites and fever
- Is there a history of coronary or peripheral vascular disease?
- Abdominal pain from an inferior MI, leaking AAA, mesenteric infarction or descending aortic dissection (with hypertension)
- Could the patient be pregnant?
- What medication is the patient currently prescribed?
- Anticoagulants, NSAIDs and steroids?
- Is there a history of abdominal pain?
Examination
| Examination | Notes |
|---|---|
| HEENT | Jaundiced sclerae ⇒ hepatitis, cholangitis, cholelithiasis |
| Spider naevi ⇒ chronic liver disease | |
| CVS | Flat neck veins and JVP ⇒ volume depletion |
| New onset of arrhythmia or mitral incompetence murmur ⇒ myocardial infarction | |
| Respiratory | Shallow respirations with restricted abdominal wall movement ⇒ localised or generalised peritoneal inflammation |
| Stony dullness to percussion, decreased breath sounds, decreased tactile vocal fremitus ⇒ basal pleural effusions | |
| Dullness to percussion, crackles and diminished or bronchial breath sounds ⇒ basal pneumonia consolidation | |
| SKin | Jaundice, spider naevi, palmar erythema, gynaecomastia, bruising ⇒ liver failure |
| Caput medusa ⇒ portal hypertension with varices |
Abdominal Examination
- Inspection
- Scars
- Abdominal distension
- Ascites
- Bruising to flanks or umbilicus (e.g. Grey-Turner”s sign or Cullen’s sign)
- Palpation
- Palpate quadrants away from point of maximal pain
- Check for guarding
- Check for rebound tenderness
- Combination of a rigid abdomen, guarding and percussion tenderness ⇒ peritonitis
- Test for shifting dullness
- Check all hernial orifices
- Percussion
- Tympanic ⇒ bowel obstruction
- Auscultation
- Tinkling bowel sounds ⇒ mechanical bowel obstruction
- Absent bowel sounds ⇒ Paralytic ileus or generalised peritonitis
- DRE with chaperone if indicated
- Pelvic exam if indicated
- Special signs:
- Murphy’s sign, psoas sign, obturator sign, rosving’s sign
Investigations
- Bedside
- Urinalysis and urine dipstick
- Blood glucose and ketones
- Beta-hCG
- ECG (especially in older patients)
- eFAST
- Bloods
- FBC (elevated WBC count supports an infectious or inflammatory aetiology, but may still be normal with acute appendicitis).
- U&E (renal function, hydration status, acidosis—low bicarbonate).
- LFTs (raised in hepatitis and biliary tract disease; may show hypercalcaemia)
- Lipase (or amylase) for pancreatitis. May not be raised in chronic pancreatitis
- Imaging
- AXR only to look for:
- Free air under diaphragm
- Dilated loops of bowel
- Calcification of gallstones or renal tract stones or pancreatic calcificiation
- Ultrasound
- CT
- Should no delay referral to surgical team especially in surgical acute abdominal pain
- AXR only to look for:
Management
Immediate Management
- IV fluids
- Analgesia
- Discussed with senior
- Requested surgical/gynae/urology/vascular review especially in hypotensive patients
- Keep NBM if acute surgical abdomen
- IV broad spectrum antibiotics (e.g. ampicillin 2g, gentamicin 5mg/kg and metronidazole 500mg) for patients with suspected infection, perforation or necrosis
Specific Management
- Bowel Obstruction
- Keep the patient NBM; insert an NGT if persistent vomiting, commence IV fluid resuscitation and give adequate narcotic analgesia
- Organise surgical review and abdominal imaging
- Ruptured AAA
- Commence fluid resuscitation with small amounts of normal saline or Hartmann’s solution (compound sodium lactate), aiming for a SBP of no more than 90–100 mmHg.
- Avoid the temptation to give massive fluid replacement, as this leads to coagulopathy, hypothermia, increased bleeding and a higher mortality.
- Contact your senior and the vascular surgeon on call urgently.
- Request a rapid bedside USS (if the patient is haemodynamically unstable) to confirm the presence of an abdominal aneurysm, or proceed directly to theatre (if the patient is moribund).
- Ensure that the patient has two large-bore IV cannulae and that blood has been sent for cross-match of 4–6 units of packed RBCs.
- Arrange a CT scan with IV contrast only if the patient’s vital signs are stable
- Perforated viscus
- Organise an immediate surgical consultation and keep the patient NBM. Arrange a CT scan to differentiate the underlying cause
- Biliary colic
- Lipase as well to assess for gallstone pancreatitis
- Upper abdominal USS
- IV fluids and IV analgesia (e.g. morphine 0.1mg/kg IV) with an antiemetic (e.g. metoclopramide 10-20mg IV)
- Low fat diet and surgical referral
- Acute cholecystitis/Ascending cholangitis
- Gain IV access, commence IV fluids and give gentamicin 5 mg/kg IV with ampicillin 2 g IV QDS
- Give analgesia such as morphine 0.1 mg/kg IV, with an antiemetic such as metoclopramide 10–20 mg IV if the patient is nauseated or vomiting
- Confirm with an upper abdominal USS
- Pancreatitis
- Keep the patient NBM, commence IV fluid resuscitation with normal saline and titrate a narcotic analgesic agent such boluses of morphine 0.1 mg/kg IV with an antiemetic such as metoclopramide 10–20 mg IV for nausea or vomiting.
- Arrange an abdominal CT scan if the patient develops fever or shock. A CT scan is diagnostic, prognostic and shows most complications.
- Refer patient to the ICU if severe pancreatitis with sepsis, abscess formation or generalised peritonitis with multiorgan failure.
- Renal calculus
- Request an urgent non-contrast abdominal CT scan of the renal tract in a patient with acute flank pain to confirm the diagnosis and rule out alternative retroperitoneal pathology.
- Or organise USS if the diagnosis is already known and pain recurs.
- Request a plain AXR (KUB) to later track the course of the calculus.
- Commence IV fluids and give morphine 0.1 mg/kg IV if the pain is intense and incapacitating, adding an antiemetic such as metoclopramide 10–20 mg IV if the patient is nauseated or vomiting. Follow up with indomethacin 100 mg PR BD, which provides excellent longer-lasting analgesia.
- Refer any patient with resistant pain, a stone >6 mm in diameter (unlikely to pass spontaneously), a stone in a unilateral kidney or a patient with any evidence of urosepsis (fever, tachycardia, hypotension and leucocytes/bacteria on urinalysis) to the urology team.
- Suspected urosepsis is a surgical emergency requiring immediate percutaneous drainage