Risk Factors
- Hypertension especially in males >60 years
- Bicuspid aortic valve
- Coarctation
- Iatrogenic (e.g. from cardiac catheterisation)
- If <40 years consider Marfan’s or Ehler-Danlos syndrome
- Cocaine use
- Known aortic valve disease or known thoracic aortic aneurysm
Presentation
- Sudden onset of severe pain that is sharp or tearing, retrosternal to interscapular and may migrate
- Pain is out of proportion to other clinical findings and difficult to relieve even with large doses of IV opioid
- ECG findings could be any of normal sinus rhythym, ischaemia (esp. inferior), non-specific ST and T wave changes or LVH
- Troponin may be elevated
Assessment
- Look for unequal or absent pulses (e.g. a difference of >20 mmHg BP between arms or other complications such as aortic regurgitation, pleural effusion or focal neurological defecit)
- Use Aortic dissection detection risk score (ADD-RS) https://www.mdcalc.com/calc/4060/aortic-dissection-detection-risk-score-add-rs
Investigations
- Echocardiography
- Transthoracic
- 75% diagnostic Type A (ascending), 40% descending (Type B) can identify complications (e.g. aortic regurgitation, regional wall abnormalities in cardiac ischaemia, cardiac tamponade)
- Transoesophageal (TOE)
- Much higher sensitivity/specificity, though operator-dependent, need sedation, and is less available
- Useful in ICU / perioperative
- Upper ascending aorta and arch not well visualised
- Transthoracic
Management
- Call senior doctor immediately if suspicion of aortic dissection
- Give oxygen to maintain saturation >95%
- Insert two large IV cannulae (14-16G) and send blood for immediate cross-match of six units packed RBCs
- Relieve pain with titrated IV morphine 2.5-5mg repeated as necessary or fentanyl PCA
- Review CXR
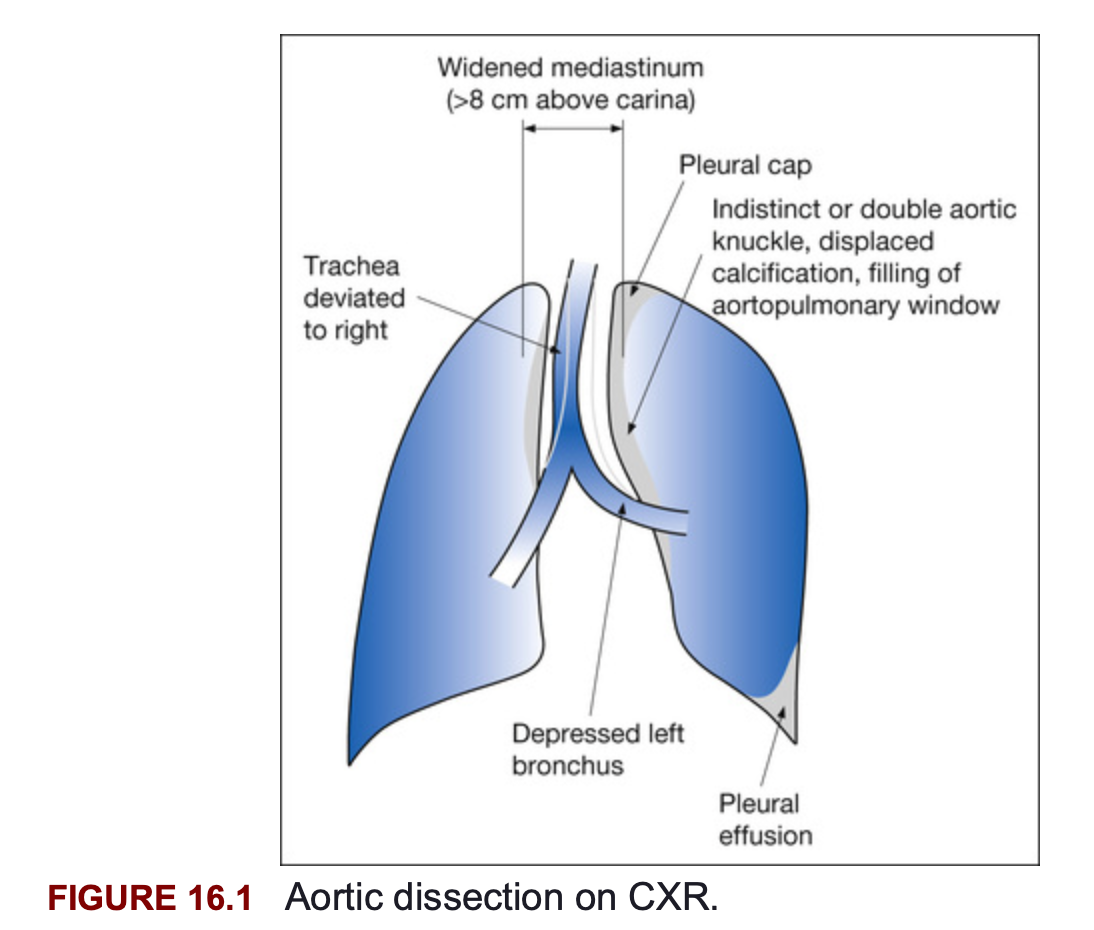
- If clinical suspicion is still high or if CXR suggestive of aortic dissection1 (AAD-RS >1):
- Arrange for urgent helical CTA of the chest or TOE
- If CTA/TOE confirms AAD → arrange admission to ICU and contact cardiothoracic or vascular surgical team
- Give IV beta-blocker such as esmolol (initial bolus of 40mg IV & infusion of 20mg/min) or labetalol (20mg IV with repeated doses of 20-40mg every 10 minutes to effect or a total dose of 300mg) or metoprolol (5mg repeated 5 minutely to a 15mg initial bolus & infusion 5mg/hr) slowly until the pulse is 60-80bpm2 or right arm SBP 100-120mmHg
- Right arm BP most likely accurate or use higher number
- Place arterial line
- In ICU with intra-arterial BP monitoring: if BP not controlled despite <60 beats/min add sodium nitroprusside or a GTN infusion until SBP 100-120 mmHg
- Correct coagulopathy
- Prepare patient for surgery if type A AAD otherwise if type B AAD manage in ICU with control of BP and consideration of endovascular stent repair
- If clinical suspicion is low but aortic dissection is in your differential list (AAD-RS ≤1)
- Exclude with a negative D-dimer if they do not have typical history, exam or risk factors; discuss with senior regarding this approach
- D-dimer should only be considered if you have already decided the patient requires aortic dissection rule out
Example
A young healthy patient with no significant medical history presents to the ED with central chest pain which radiates to the back. The onset was not abrupt or severe and the pain is not described as ripping or tearing. He was no risk factors or exam findings suggestive of dissection. You can find no explanation for his pain and feel aortic dissection needs to be excluded. For this patient ADD score is 0 and exclusion of a dissection with a D-dimer is appropriate.
Sources
- FRCEM AFTBAFFF, FFSEM MCMMbcF, FACEM ACMMc. Marshall & Ruedy’s On Call: Principles & Protocols. 3rd edition. Elsevier; 2016. 648 Chapter 16: Chest Pain p. 117
- Emergency Care Institute Aortic Dissection https://aci.health.nsw.gov.au/networks/eci/clinical/tools/cardiology/aortic-dissection
- Aortic dissection - EMCrit Project Accessed 25/12/2025
- Acute Aortic Dissection • LITFL • CCC Cardiology Accessed 25/12/2025